Case Study: Knee Arthroscopy: The Tear of
Medial Meniscus of knee in a 46 year-old female
An injury to the medial meniscus, a piece of cartilage on the inside (inner aspect) of the knee, is known as a medial meniscus tear. More frequently than lateral meniscus injuries, medial meniscus injuries can cause locking, catching, or buckling as well as pain, stiffness, and edema. In severe circumstances, it might progress to chronic knee issues like arthritis.
After being involved in a car accident, a 46-year-old female patient came to visit a doctor at the office and complained of pain on the inside of her right knee. Her conventional medical care failed. A vertical radial tear of the medial meniscus of the right knee was discovered by MRI.
We spoke about our alternatives for treatment and decided on surgical treatment. Infection, hemorrhage, damage to the nearby nerves and blood vessels, failure to heal, need for repeat surgery, development of arthritis, and eventual need for knee replacement were just a few of the dangers and problems we covered.
We talked about several systemic issues, such as blood clots, cardiac, pulmonary, and neurological issues. The patient read the consent carefully and signed it.
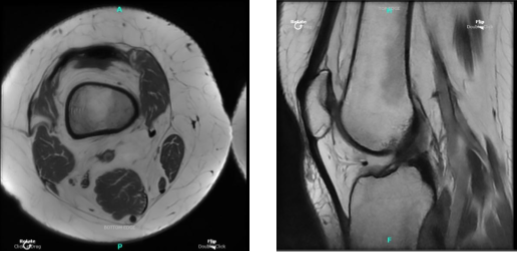
MRI Right knee non-contrast
The patient was brought into the operation room and set down on a comfortable operating table. Anesthesia was induced throughout. An antibiotic was given before surgery. The right lower extremity was prepared as normal and dressed aseptically. A break was announced.
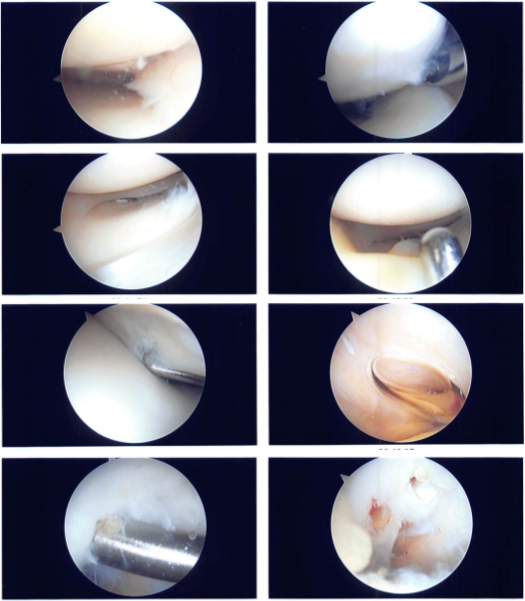
An arthroscope was inserted following the creation of a lateral entrance portal. A spinal needle was used to create the medial entrance portal. Intact cartilage was visible upon examination of the patellofemoral compartment.
An examination of the medial tibiofemoral compartment revealed a vertical radial tear along the body of the medial meniscus that extended up to the capsule. The intercondylar notch examination revealed an undamaged ACL.
The meniscus and articular cartilage were found to be intact upon examination of the lateral tibiofemoral compartment. After a meniscectomy, the decision was made to restore the meniscus due to its large size and potential inadequacy.
With the use of a razor, the meniscus’ edges were trimmed. Opposing the meniscus was simple. The choice was made to restore the horizontal mattress. Prior to using Fast-Fix x2 to pass horizontal mattresses x2, NovoStitch was utilized to pass horizontal mattresses.
The meniscus was fixed with the use of three stitches. The apposition was successful. Using chondroplasty picks, microfracture chondroplasty was carried out in the intercondylar notch. It was possible to visualize fat globules venting from the microfracture locations.
The meniscus will be able to repair as a result of the entry of bone marrow. There was a thorough irrigation and drainage of the knee. Final images of the same were captured. 3-0 nylon was used for the closure.
The knee was then given 20 mL of 0.5% Marcaine injection. Wraps made of 4×4, ABD, Webril, and Ace were used for dressing. It was put on to immobilize the knee. The patient was transported to recovery in a stable state after being extubated.
Intraoperative photo
The patient visits the office for her postoperative visit. She is using crutches and is having difficulty with braces, she is NWB Rt LE and has denied fever, chills. After one week the patient is seen by the doctor for his post operative consultation, no x-rays are needed.
His pain is well controlled, he denies fever or chills and he is using the shoulder immobilizer. We chose to proceed with official physical therapy as well as a home exercise regimen for shoulder rehabilitation after examining treatment choices.
During the visit, we removed the stitches. We will continue to use ice and elevate the shoulder to reduce swelling and pain. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications.
We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress. The patient’s progress and development have been undeniable with continued physical treatment and regular attendance at his follow-up checkups.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.