Case Study: Knee Arthroscopy: Meniscectomy including
Chondroplasty of the right knee in a 50 year-old male patient
Both meniscectomy and chondroplasty are medical treatments used to treat knee injury. Chondroplasty is a surgical procedure that involves reducing unstable cartilage flaps in order to smooth degenerative cartilage and stabilize chondral defects.
Meniscectomy is a popular orthopedic treatment used to relieve knee discomfort by cutting the unstable flaps of a torn meniscus and establishing a stable remnant meniscus.
A 50-year-old male patient visited the office for follow-up but he complained about the pain in his right knee. He also has scars on bI UL from MVAs. Upon examination of the lumbar spine, the patient is tender to palpation over the paraspinal musculature, (the paraspinal musculature, these are the muscles that surround and attach to the spine and the one that responsible for moving and stabilizing the spine, it has a vital role to work properly the spine and the body).
They are nontender over the spinous processes and have no crepitus with ranging, but it has limited ROM of the spine due to discomfort.
It also has a negative straight leg raise test and a non-tender to palpation over the trochanteric bursa and hip. It has no soft tissue swelling and ecchymosis, the patient has full range and stable motion of the hips. They have 5/5 strength, and are neurovascularly intact distally. It has no erythema, warmth or skin lesions present.
The cervical spine of the patient is the same with the lumbar spine, the difference is that the negative Spurling’s test, it is sat with the scapular protracted and depressed.
It is tender to palpation over the trapezius and rhomboids, also the clavicle and elbow. The patient has full range and stability of motion of the shoulders and have 5/5 strength, and are neurovascularly intact distally.
As the continuation of the examination, the left knee of the patient, Wound CDI and have 5/5 strength, and neurovascularly intact distally. It has no erythema, warmth or skin lesions present.
While the patient’s right knee has tender palpation along the medial and lateral joint line. They are nontender to palpation along the medial and lateral facets of the patella. He has discomfort with McMurray’s maneuvers, and the knee is stable.
In the medical history, the patient was undergone through post partial meniscectomy, medial; partial meniscectomy, lateral; chondroplasty, medial femoral condyle; chondroplasty, patellofemoral joint; Depo-Medrol injection to the knee performed a month ago, a done surgery in his right brachial plexus injury and left wrist arthrodesis. He’s also been using a Weight Bearing as Tolerated (WBAT) with a single crutch and doing PT.
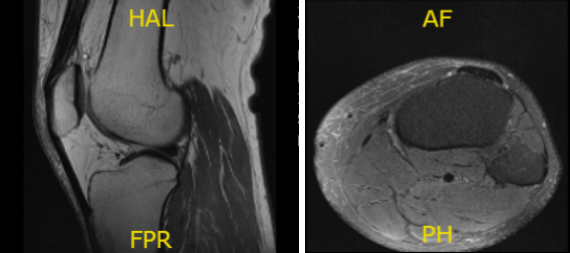
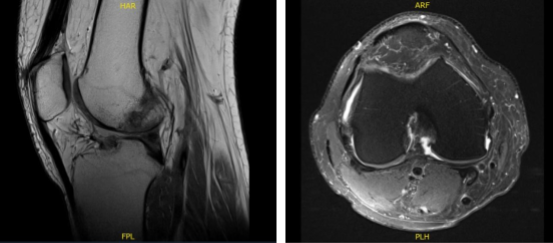
MRI presented and reviewed by the doctor. It showed that the left knee of the patient is intact in medial and lateral meniscus and has no acute osseous injury but has small joint effusion. The central trochlea has a focal chondral fissure and fibrillation in the midportion of the medial femoral condyle.
However, the right knee of the patient, prior partial lateral meniscectomy with diminutive anterior horn with a re-tear in the body of the lateral meniscus. Because of the extrusion of the body the lateral meniscus causes too mild to moderate tricompartmental osteoarthritis with small joint effusion.
The left knee x-ray that completes with patella shows that there are no acute fractures and significant degenerative changes while the right knee has no fractures but have mild osteoarthritic degenerative changes.
After the results were found, the attending physician discussed the treatment options for the patient’s diagnosis of the right knee, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. The doctor talked about the nature and purpose of the treatment along with the expected risks and benefits.
The patient expressed a desire to proceed with the surgery, the doctor educated the patient regarding the inherent and an inevitable risk that may occur, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death.
The doctor also explained to him the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome.
The possibility of not being able to alleviate all of the discomfort and there is no guarantee that the strength or it will function normally. The patient comprehends that there is a long rehabilitative process that typically follows the surgical procedure and the risks of re-tear or failure to heal.
He also understands implants may be utilized during the surgery. However, he still chooses to undergo the operation even he knows how risky the surgery was.
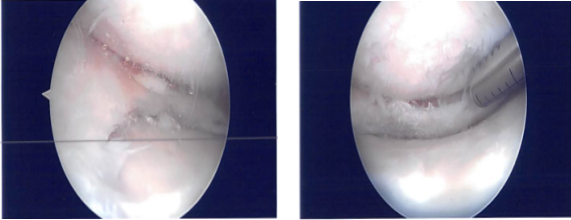
General anesthesia was induced on the patient, low thigh tourniquet was applied on the left thigh. A separate draping and dressing debris were performed and a lot of debris was found in the knee joint. There was patellofemoral arthritis.
There was fraying of the inner edge of the medial meniscus. There was OA grade 1 to grade 2 damage on the femoral condyle. The meniscus was debrided to a stable margin. A chondroplasty was performed in the medial femoral condyle.
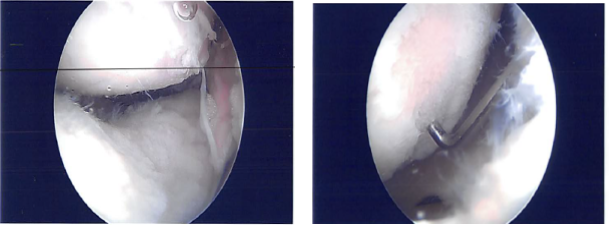
The scope was entered to the intercondylar notch and entered in the lateral femoral condyle and found fraying of the inner margin of the lateral meniscus along with the small tear. Partial meniscectomy of the inner edge was performed.
Attention was focused on the patellofemoral joint where there was osteochondral damage, grade 1 to grade 2 on the medial articular surface of the patella. It was debrided to a stable margin. There was a large osteochondral damage, grade 2 to grade 3 over the trochlea, which also debrided. Final pictures were taken.
After a week, the patient presented with discharge from the right knee with minimal pain. After two weeks post-surgery of the right knee with minimal pain, Keflex 500 mg was given to take as pain meds that he needed.
He was also advised to use WBAT and range to comfort and has decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient will use crutches, CPM and cold therapy pack. Patient had removed the sutures himself and placed steri strips on the wound.
After another week of treatment, he is doing better but has not yet started with PT of the right knee. His left knee is doing well and has achieved good ROM. No discharge, fever, chills. Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
