Case Study: Knee Arthroscopic: Medial Meniscectomy
in a 68 year-old male
A meniscectomy, a form of arthroscopic knee surgery, is the surgical excision of a damaged meniscus. Your meniscus acts as a knee cushion and distributes your weight evenly so that your knee remains stable.
A 68-year-old male patient presents right knee pain, he states he had knee surgery for medial meniscus tear and is still having pain and wants a second opinion. He is here with an MRI of the knee. We discussed treatment options and opted for surgical management.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, reinjury, repeat surgery, need for total knee replacement, need for rehabilitation among others. We discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications among others. The patient understood and signed an informed consent.
MRIs were reviewed and discussed by the doctor; we discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options.
We also discussed the nature and purpose of the treatment options along with the expected risks and benefits. The patient has expressed a desire to proceed with surgery, and we think that is a reasonable option.
We educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
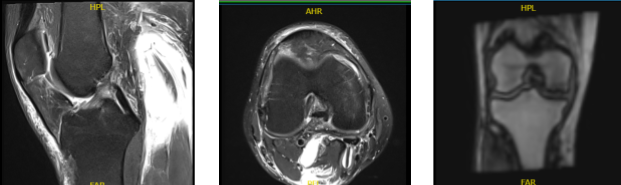
MRI Right Knee Non-contrast
Examination of the menisci reveals a tear of the posterior horn of the medial meniscus with abnormal signal within the posterior horn which contacts the inferior articular surface. No tears are seen within the lateral meniscus. The anterior and posterior cruciate and medial and lateral collateral ligaments appear intact.
The patellar and quadriceps tendons appear intact. There is a small joint effusion. The distal femur, proximal tibia and fibula, and patella appear intact without evidence of any fractures, contusions, or bony lesions. The popliteal fossa is clear. There is prepatellar and pretibial soft tissue edema.
The patient was taken to the operating room where he was placed on the well-padded operating table. General anesthesia was induced. Preoperative antibiotics were given. Low-thigh tourniquet was applied. Time-out was called. Right knee was prepped and draped aseptically in usual fashion.
Anterior portal was made through a lateral parapatellar incision. Arthroscope was inserted. Medial anterior portal through the medial parapatellar incision with the use of spinal needle was then made.
Examination of the medial tibiofemoral compartment showed horizontal tear along the posterior horn of the medial meniscus with status post meniscectomy. There was a healing articular defect of grade 2 to grade 3 of the medial femoral condyle. Examination of the intercondylar notch showed intact, but degenerative ACL.
Examination of the lateral tibiofemoral compartment showed intact meniscus and intact cartilage. Examination of the patellofemoral compartment showed intact cartilage. A shaver was used to perform meniscectomy, followed by up cutting and right angled biters. Final shavings were done with the use of the shaver again. was removed.
The knee was thoroughly irrigated and drained. Pictures were taken and saved. Then 20 mL of 0.5% Naropin mixed with 40 mg of Depo-Medrol was injected into the knee. Closure was done with the use of # 3-0 nylon. Dressing was done with the use of Adaptic, 4 x 4s, Webril and Ace wrap. The patient was extubated and moved to recovery in stable condition.
He is here for his postoperative appt today, no x-rays were needed. Denies fever, chills and pain is well controlled. He does develop pain after walking and stairs. We have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We removed the stitches during the visit.
We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in three weeks’ time to evaluate their progress. They will call us in the interim if they have any questions or concerns prior to their follow up visit.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling. After a sterile prep, 7cc of 1% Lidocaine and 80mg of depo-medrol were injected into the right knee.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail. With regular visits in the office, the patient did well after the surgery and continued physical therapy for the knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
