Case Study: Left Knee Arthroscopy: Medial Meniscus Root
Repair and Lateral Meniscectomy in a 57 year-old Patient
The procedure for repairing a meniscus root entails separating the root, stitching at least two sutures into the remaining meniscal connection, and attempting to realign the root to a more anatomic position.
The posterior horn of the meniscus may occasionally need to be freed from scar tissue so that it can be relocated. There are several indications and symptoms of knee arthritis, including: sounds that crackle, click, grind, or snap (crepitus). walking challenge. joint discomfort that fluctuates with the weather (gets better or worse).
A 57 year-old patient was in our office with complaints regarding left knee pain. She went skiing and she felt twisting her left knee. She did not seek medical treatment until today. The severity of the pain is 4/10.
She states the pain is mild and has gotten better since Friday. If she is walking and her leg goes a certain way, she feels more pain. After she sits for a while and stands up the pain is worse. She stated her knee is swollen and the pain is more on the side.
She presented X-ray which showed no fracture or post fracture deformity. Preserved joint spaces. No osteophytes or erosions. Unremarkable soft tissue structures for both knees.

X-ray Bilateral Knees 3 views each
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. I also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
I also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
I talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. I discussed the type of implants that may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. I discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. I have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. Preop antibiotic was given. Left lower extremity was put in a C-clamp after application of the tourniquet.
The left lower extremity was prepped and draped aseptically in usual fashion. Preop antibiotic was given. Esmarch was applied and tourniquet was elevated. A lateral entry portal was made with a transverse parapatellar incision. Arthroscope was inserted.
Examination of the patellofemoral joint showed grade 1-grade 2 osteoarthritic changes at the patella more than trochlea. The arthroscope was moved to the medial tibiofemoral compartment where a medial entry portal was made with the use of a spinal needle.
Examination of the medial tibiofemoral compartment showed grade 1-grade 2 osteoarthritic changes of the medial femoral condyle which was cleaned with the use of shaver. It also showed the tear of the medial meniscus root. Rest of the meniscus was healthy. We made a decision to repair the meniscus.
FiberWire sutures were used to pass through the root x 2. Meniscus root repair jig from Arthrex was used to drill a hole through a separate incision. A 70-degree angle was used. The slit was passed down to the bone and a FlipCutter was used to drill a hole of about 5 mm from the posterior margin.
Once the FlipCutter was in, it was flipped and a 5 mm gutter was made for the meniscus to sink in. A passing loop was passed through the tunnel and retrieved. The FiberWire were passed through the passing loop unto the tunnel and brought out near the tibial tuberosity. A good reduction of the meniscus would be seen and pictures were taken and saved.
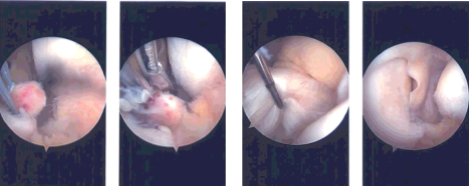
Intraoperative Arthroscopy Images
The sutures were ported into the tibia with the use of a 4.75 SwiveLock after drilling and tapping. A good reduction and fixation of the meniscus root was achieved. Examination of the intercondylar notch showed an intact ACL. E
xamination of the lateral tibiofemoral compartment showed intact cartilage but there was a medial free margin tearing of the lateral meniscus, which was cleaned with the use of a shaver. Balanced margins were achieved.
Examination of the patellofemoral compartment showed grade 1-grade 2 osteoarthritic changes in the patella more than trochlea. Shaver was used to shave the arthritic changes to a balanced margin. Knee was thoroughly irrigated and drained.
Closure was done with the use of # 3-0 nylon. 10 cc of 0.5% ropivacaine was injected into the knee. Dressing was done with the use of Xeroform, 4×4, ABD, Webril, and Ace wrap. Knee immobilizer was applied and locked in extension. The patient was extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
