Case Study: Knee Arthroscopic: Medial Meniscus Root
Repair, Lateral Meniscectomy and
Chondroplasty in a 66 year-old patient
Meniscus root repairs are done by isolating the root, stitching at least two sutures into the remaining meniscal connection, and then attempting to move the root back into a more anatomic position. The meniscus posterior horn may occasionally need to be freed from scar tissue.
The tibia and femur may begin to inappropriately rub together without this meniscus cushion. This may eventually result in ongoing knee discomfort. It could eventually lead to arthritis. Your “cap” of cartilage deteriorates, causing the bones below to rub against one another.
A 66-year-old patient was in our office with complaints regarding left knee pain. She has been experiencing this pain for a month. She denies any injury to the knee. She went to her PCP who recommended x ray showing bone on bone. She presented an Xray result that showed no significant degenerative changes.
There are no acute fractures. She also presented an MRI results that showed trace joint effusion. Tiny popliteal cyst. Minimal lateral patellar shift. Degenerative medial and lateral meniscus tears as detailed above. Minimal osteoarthritis in the medial and lateral joint compartment of the left knee.
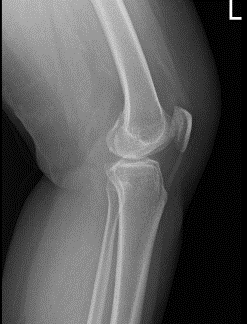
Left Knee X-ray AP and Lateral with Oblique 3 views
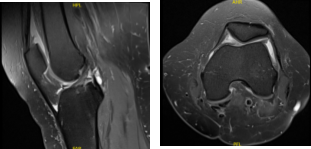
MRI Left knee non-contrast
We discussed treatment options and opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, need for repeat surgery, need for rehabilitation, development of arthritis and need for knee replacement in the future, systemic complications including blood clot, cardiac, pulmonary, neurological complications among others.
The patient understood and signed an informed consent. The patient was taken to the operating room where an adductor canal block was done by the anesthesia team. General anesthesia was induced. The tourniquet was applied over the thigh.
The left knee was prepped and draped aseptically in a usual fashion. Preop antibiotic was given. The limb was exsanguinated and the tourniquet was elevated. A lateral entry portal was made with the use of a knife. An arthroscope was inserted. Examination of the patellofemoral compartment showed intact cartilage.
The medial entry portal was made with the use of spinal needle under visualization. Examination of the medial compartment showed medial meniscus root tear, which was hanging over the flimsy tissue to the capsule, which could easily be freed. Decision was done to medial meniscus root repair.
Arthrex medial meniscus root repair was used and was inserted (3:18) with incision was given on the tibia (3:20) was inserted. A FlipCutter was inserted through the (3:23) and was brought out to the posterior tibial plateau in the region of the meniscus root.
The FlipCutter was flipped so as to ream to about 5 mm to make a trough for the root. A wire was used to keep the canal patent. Now, FiberLink x2 were passed through the root with the use of labral scorpion. They were passed down through the tunnel and brought out onto the tibia. Root was found to be in a good position onto the bone.
The sutures were tied onto each other over a button. After the repair of the suture, it was found that the roots were not opposed to the bone, so a decision was made to put 4.75 SwiveLock, which was inserted after preparing the hole with a sutures passed through it. A good reduction and repair of the medial meniscus was achieved.
Examination of the intercondylar notch showed intact ACL. Examination of the lateral compartment showed partial tearing of the lateral meniscus, which was debrided with the use of shaver. Final pictures were taken and saved.
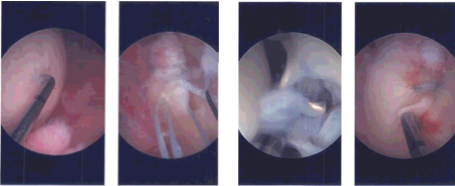
Intraoperative Arthroscopy Images
Closure was done with #3-0 nylon. Dressing was done with the use of Xeroform, 4×4, ABD, Webril and Ace wrap. Knee immobilizer was applied and the patient was extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
