Case Study: Arthroscopic Lateral Meniscectomy and
Chondroplasty of the Left Knee in 47-year-old Female
The patient is in our office, with complaints of left knee pain for the last 6 months. She first experienced knee pain while working at a gym as an instructor. The patient has been on and off at work secondary to pain. The pain is moderate in intensity. The pain is constant. The pain is associated with swelling.
The pain is not associated with bruising, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or limping, hand function difficulty. The problem has been getting unchanged since it started. Navigating stairs, bending, kneeling make the symptoms worse.
Rest, Ice, and ace bandage make the symptoms better. The patient has had right knee surgery (ACL recon and patellar microfracture) 10 years ago. The patient is allergic to penicillin. The patient is right-handed. The patient does not smoke. Her current medications include Budecort inhaler for asthma, Ibuprofen for pain, Hydrochlorothiazide for hypertension, and atorvastatin for hyperlipidemia.
Upon examination of the left knee, the patient has mild effusion. Positive lateral joint line tenderness. There is no pain with the manipulation of the patella. There is no crepitation with passive or active range of motion. There is no medial joint tenderness.
McMurray’s maneuver is positive for lateral joint line tenderness. Collateral ligaments are intact. Lachman’s test negative. Anterior drawer and posterior drawer negative. There is no soft tissue swelling distally. The neurovascular examination is intact.
On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
MRI of the left knee suggested a lateral meniscal tear.. There was mild partial-thickness cartilage loss along the central trochlear groove and in the lateral compartment.

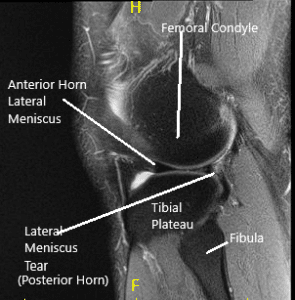
MRI of the Knee in coronal and sagittal sections
The results of the MRI were discussed at length with the patient. Various treatment options including surgical and non-surgical were discussed with the patient at length. The patient decided to go ahead with the arthroscopic surgery.
PREOPERATIVE DIAGNOSIS: Lateral meniscus tear of the left knee.
POSTOPERATIVE DIAGNOSES:
- A lateral meniscus tear of the left knee.
- Osteochondral lesion grade 3 to grade 4 in the trochlea.
- Grade 1 to grade 2 osteochondral lesions of the lateral femoral condyle.
OPERATION:
- Left knee Lateral meniscectomy.
- Left knee Microfracture of the trochlea.
- Left knee Chondroplasty of the lateral femoral condyle.
PROCEDURE: The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. The left lower extremity was put in a tourniquet and prepped and draped in an aseptic usual manner. A time-out was called. A preoperative antibiotic was given. Tourniquet was elevated. A lateral entry portal was made and the scope was introduced.
The patellofemoral joint was checked. The posterior surface of the patella was pristine, but there was a large grade 3 to grade 4 osteochondral lesions in the trochlea. The medial meniscus was checked and found to be intact. The medial femoral condyle was good. Lateral meniscus showed a tear in the posterior body of the lateral meniscus vertical radially oriented up to the periphery. There was a grade 1 to grade 2 osteochondral lesions on the lateral femoral condyle also.
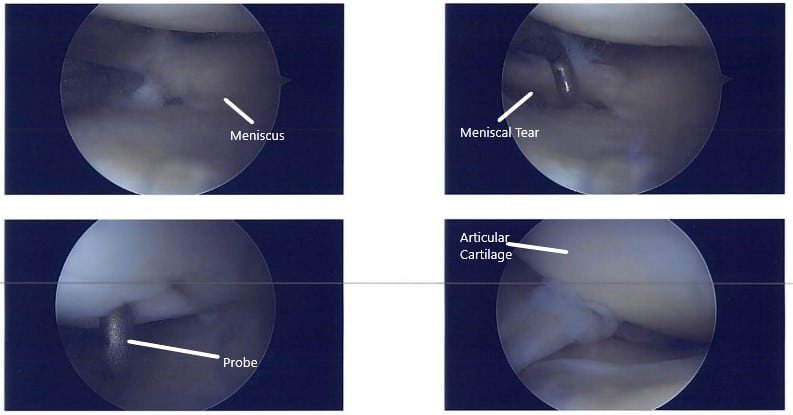
Intraoperative arthroscopic images.
A medial entry portal was made with direct access to the lateral meniscus. A shaver and up biters were introduced and the meniscectomy was performed as the meniscus was not amenable to repair. Stable margins were reached. The chondroplasty of the lateral femoral condyle was done. The chondroplasty of the trochlea was also done and considering it to be a grade 4 lesion. A microfracture was performed. Fat globules could be seen coming out.
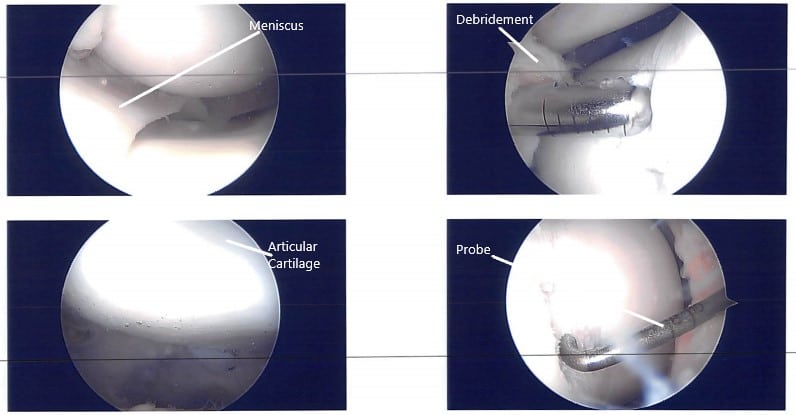
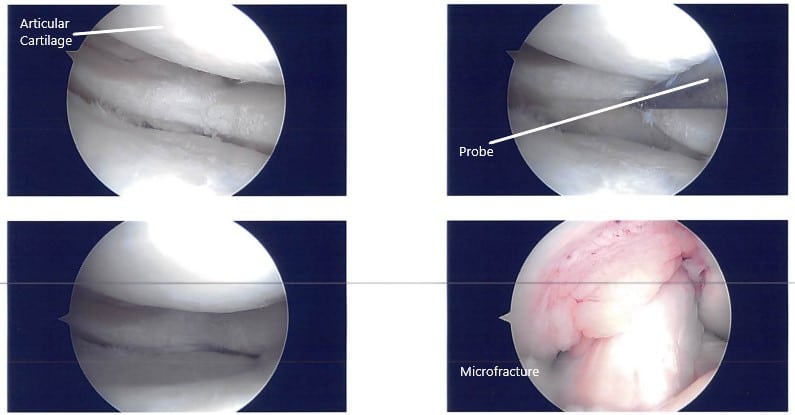
Intraoperative arthroscopic images.
The knee was copiously washed. The closure was done using nylon #3-0. A 20 cc of Naropin 0.5% was injected. The dressing was done. The patient was moved to the holding area from the postoperative care unit in a stable condition after extubation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
