Case Study: Knee Arthroscopy: Medial Meniscectomy
and Chondroplasty in a 55 year-old man
Arthroscopy blades and shavers are combined to conduct partial meniscectomy. At three weeks after surgery, you can swim as long as the incisions are fully healed. After two to three weeks after surgery, you can play golf.
For a few weeks, kindly refrain from overdoing the knee pivoting or twisting. You can return to play for the majority of contact sports 2-4 weeks after surgery. Long-term swelling and discomfort in the knee joint are possible, and the leg’s thigh muscles may weaken and tone down significantly.
To hasten your recovery and safeguard your future joint function, a specialized exercise regimen and rehabilitation program may be advised.
The patient, a 55-year-old man, complained of pain on the inside of his right knee when he was examined by me at my clinic. He did not respond to conventional therapy. An MRI we obtained revealed a medial meniscus tear with potential root involvement.
The patient chose surgical treatment after we had a discussion about his or her options. Infection, bleeding, nonhealing, the need for repeat surgery, arthritis aggravation, knee rehabilitation, the need for cortisone injections versus surgery, systemic complications like blood clots, cardiac, pulmonary, and neurologic complications including death were among the risks and benefits we discussed. The client was aware and gave informed consent.
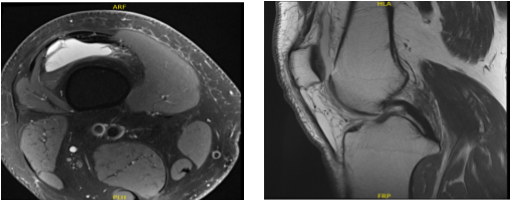
MRI-3T right knee non-contrast
In the operating room, general anesthesia was produced on the patient. An antibiotic was administered before surgery. The right lower extremity was prepared as normal and dressed aseptically. The tourniquet was put on. A timeout was ordered. The tourniquet was raised and Esmarch was administered.
An arthroscopic entrance portal can be performed through a lateral entry portal. The user sat down inside the arthroscope. Grade 1 to grade 2 osteochondral lesions of the lateral aspect of the patella were discovered during a patellofemoral examination.
A medial meniscus tear was evident upon examination of the medial compartment. A spinal needle was used to create a medial entrance hole. When the probe was inserted, an evaluation of the medial meniscus tear revealed a lateral border tear with a flap.
The root remained unaffected, however there was a tear that went all the way to the posterior horn. The choice was made to remove the medial meniscus. Biters were used to conduct the medial meniscectomy, then shavers. A favorable margin was attained.
An intact ACL was visible upon examination of the left intercondylar notch. Both the lateral meniscus and the lateral femoral cartilage were seen upon examination of the lateral compartment. Additionally entered was the medial femoral cartilage.
A grade 1 to grade 2 osteochondral lesion was discovered during the patellofemoral examination and was removed with a razor. The medial entrance portal was used to insert the arthroscope, which was then used to balance the medial meniscus and perform chondroplasty using the shaver.
Final images were captured and stored. It was irrigated and drained completely on the knee. #4-0 nylon was used for the closure. The knee was then injected with 9 cc of 0.5% Naropin and 40 mg of Depo-Medrol. ABD, Webril, Xeroform, and Ace wrap were used for dressing. The patient was transported to recovery in stable condition after being extubated.
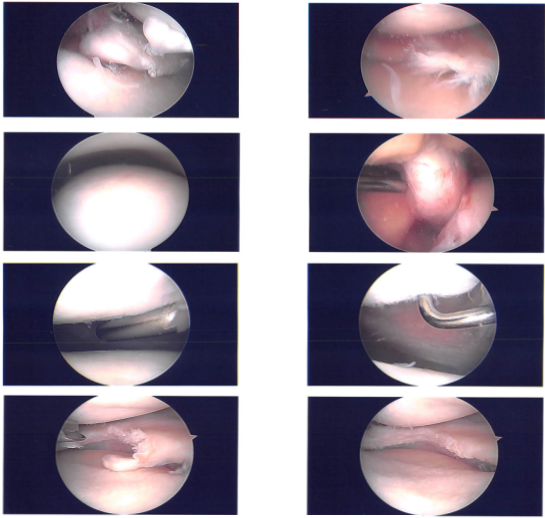
Clinical photo
The patient came today for his one week post operative consultation, no x-rays were needed. He is doing well though, he is using a cane occasionally. He has started PT. His left foot pain is bothering him.
We have decided to move through with official physical therapy as well as a home workout regimen for knee rehabilitation after discussing our treatment choices. During the visit, the stitches were taken out and the arthroscopic images were reviewed.
We’ll keep applying ice and elevating the knee to reduce discomfort and swelling. To lower the risk of a deep vein thrombosis, we shall keep using mechanical prophylaxis and early mobilization.
As long as there are no contraindications to these medications, we will wean them off of any narcotic medications before switching them to anti-inflammatories and Tylenol. We also talked about the advantages, disadvantages, and typical adverse effects of using these medicines.
In three weeks, the patient will return to assess their progress. Planned to have an MRI of my left foot in the next visit.
The patient came to the office after a month for his post operative visits, he is doing well. He has started PT though; his left foot pain is still bothering him. He got a second shot in left foot with a different podiatrist which had helped him tremendously.
His knee pain is also resolved. He is walking unaided without limp or discomfort. The patient’s progress and development have been undeniable with continued physical treatment and regular attendance at his follow-up checkups.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
