Case Study: Management of Bilateral Hip Avascular Necrosis (AVN)
in a 56-year-old female with Lupus Nephritis
A 56-year-old female presented with complaints of bilateral groin pain. The pain was first noticed six years back and gradually progressed over the years. There was an associated stiffness in both hips. The patient was a known case of lupus nephritis on steroid treatment for the last ten years.
The pain was mild initially but had progressed in severity. The pain was described as a dull ache and was not associated with any radiation. The patient stated that the pain was constant and disturbed her sleep.
She had an exacerbation of hip pain with climbing stairs, walking, prolonged standing, bending, squatting and getting up from a chair. The pain was only temporarily relieved with analgesics. She was a school teacher currently not working.
She was able to walk only for three blocks without pain. She used a cane as an assistive device for walking. Recently, she experienced severe disability in performing even simple tasks such as taking a shower or getting up from a toilet seat.
She was a nonsmoker and a nondrinker. She previously had a hysterectomy 15 years ago. She was currently on steroids, Zoledronic acid, Losartan and Spironolactone.
On physical examination, there was no evidence of exaggerated lumbar lordosis or scoliosis. The patient walked with an antalgic gait. The bilateral shoulders, iliac spines, patella, and malleolus were at the same levels.
There was no evidence of any wasting of the gluteal or thigh muscles. Tenderness was present on the bilateral anterior hip joint line. There was no evidence of inguinal lymphadenopathy in both hips. The skin overlying both the groins was normal with no evidence of scar marks or sinus tracts.
There was no leg length discrepancy and both the trochanter was at the same level on digital palpation. The range of motion of both the hips was restricted especially in internal rotation and abduction. There was a differential rotation of both the hip joints on hip flexion.
There was no evidence of distal neurological deficit. The bilateral lower extremity pulses were palpable and comparable. The examination of bilateral knees and ankles was normal. The power and sensory examination of both the lower extremities was normal. The deep tendon reflexes were present and comparable bilaterally.
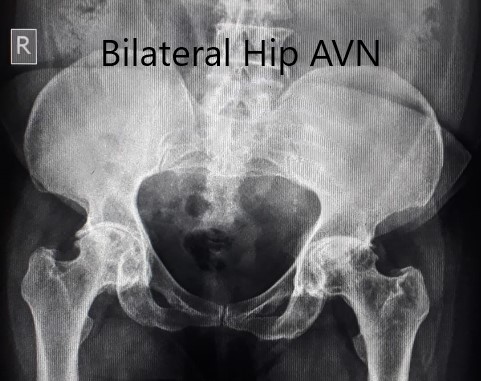
Preoperative X-ray of the pelvis in anteroposterior view.

Pre-operative X-ray of the pelvis in frog-legged lateral views.
An X-ray was obtained which suggested a deformed head of femur bilaterally. There were features of arthritis bilaterally with joint space reduction, sclerosis, subchondral cysts, and osteophytes bilaterally.
MRI was obtained which showed:
Right Hip Joint: There is a loss of sphericity of right femoral head, involving more than 2/3 of the circumference. In the superior part of the right femoral head, a focal lesion is visualized which is bounded by a serpiginous T1 hypointense margin. The lesion is hypointense on both T1 & T2WI relative to the marrow (Mitchell class – D).
No subchondral fracture is detected. A minimal amount of fluid is seen in the joint cavity. The femoral neck and acetabulum display normal signal intensity. Muscles in view display normal signal intensity.
Left hip joint: Displays similar although less severe changes. The sphericity of the left femoral head is maintained. There is more than 2/3 circumferential involvement of the left femoral head. No subchondral fracture is seen. No joint effusion is seen.
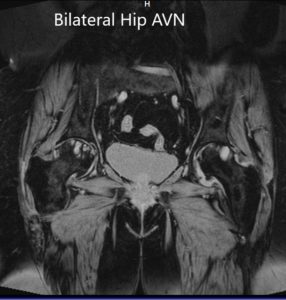
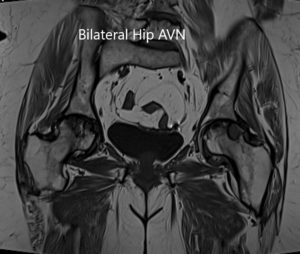
Coronal section of T2WI and T1WI of pelvis MRI.

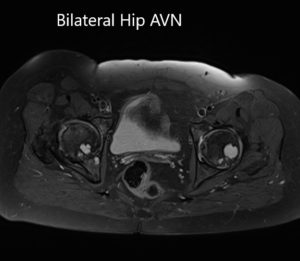
Axial sections of T1WI and T2WI of the pelvis MRI.
The patient had bilateral avascular necrosis of femoral heads with acetabulum involvement. The patient was advised bilateral total hip replacement. Risks, benefits, and alternatives were discussed with the patient at length. She agreed with the plan.
She underwent a bilateral total hip replacement. Postoperatively the pain was managed with medications. Aspirin was prescribed for prophylaxis of deep vein thrombosis. The sutures were removed uneventfully.
Weight-bearing was allowed as tolerated with support. Hip precautions were advised and the physical therapy was started to increase strength and flexibility.
Three months post-op the patient was able to walk without support. The range of motion was excellent and the patient reported zero pain. The patient was extremely happy with the outcome and was able to get back to her baseline very quickly. She was back at her job and follows up as needed.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
