Case Study: Open Reduction and Internal Fixation
of Right Distal Radius in a 58 year-old patient
A damaged bone can be stabilized and healed using a procedure called open reduction and internal fixation (ORIF). This treatment could be required to fix a fractured fibula or shinbone. The bigger bone in your lower leg is called the tibia, or shinbone.
Years later, arthritis can be brought on by fractures that extend into a joint. Long after taking a break, if your wrist begins to pain or swell, contact your doctor for a checkup. blood vessel or nerve injury. A wrist injury has the potential to harm nearby blood vessels and nerves.
The 58-year-old patient was in our office with complaints of right wrist pain. She slipped and fell landing on her right wrist. The pain is severe in nature. She describes the pain as stabbing and throbbing.
She states her fingers are numb, but she denies any tingling. She is taking pain medication. During the visit, the patient presented X Ray results from Long Island Community Hospital which showed fractures of the distal radius and ulnar styloid.
The patient presented results for CT scan that showed acute-to-subacute intra-articular fracture of the right distal radius as detailed above. Companion fracture of the ulnar styloid as noted. Small joint effusions. Chondrocalcinosis as detailed above.
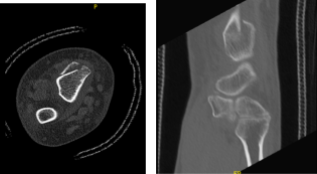
CT Right wrist non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. I also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
I also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
I talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. I discussed the type of implants that may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. I discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. I have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating table. Supraclavicular block was given. General anesthesia was induced. Right upper extremity was prepped and draped aseptically in usual fashion after application of tourniquet. Time-out was called.
Esmarch was applied and tourniquet was elevated. A Bruner incision was planned. Preop antibiotics were already given. A Bruner incision was given along the sheath of the flexor carpi radialis. Hemostasis was achieved. The anterior sheath of flexor carpi radialis was cut in line of incision.
The tendon was retracted medially. Posterior sheath was also cut in the line of incision. Pronator quadratus was seen and was reached from the radial border. Hemostasis was achieved. The fracture was seen healing. An osteotome was used to achieve osteoclasis.
The fracture was reduced and held with a volar plate and olive wires. The distal segment was fixed to the plate with the use of two cortical screws, which were later wasted. The plate was proximally fixed with one cortical screw.
The distal fragment was fixed to the plate with the use of locking screws x5 followed by change of the two cortical screws with two more locking screws. The proximal plate was fixed with the use of nonlocking screws. Rotational fluoroscopy and all the screws were found to be in an acceptable position.
The distal forearm was in good alignment. There were some dorsal openings which were accepted. Wound was thoroughly irrigated and drained. Hemostasis was again achieved. Closure was done with the use of # 2-0 Vicryl for pronator quadratus followed by #2-0 Vicryl for subcuticular layer.
Dressing was done with the use of Dermabond followed by Adaptic, Webril. Short arm splint was applied, and Ace wrap was applied. Tourniquet was released. The patient was extubated and moved to recovery in stable condition. Shoulder sling was applied.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the wrist. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her wrist.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
