Case Study: Knee Arthroscopy: Medial and Lateral
Meniscectomy to a 50 year-old male railroad worker
Knee arthroscopy is a crucial diagnostic and therapeutic tool for the therapy of knee diseases. Examples of indications include meniscectomy, removal of loose bodies, chondroplasty, microfracture, irrigation and debridement, and tendon reconstruction. In this series of essays, we thoroughly examine the medial and lateral meniscus of a male worker who used his knee strength all the time.
Because of their frequent motion and use of the knee, railroad workers may develop knee injuries. One of the most frequent ailments to the knee is a torn meniscus. A torn meniscus can result from any abrupt twisting or rotating of the knee, particularly if you are bearing all of your weight on it.
Patient is here today with a complaint of left knee pain that started two months ago. The patient stated that while working on the Long Island Railroad, he was stepping down off of the train and felt his knee buckle and twist. He then presented to the Urgent Care where he was sent for x-rays.
The patient reports pain as moderate to severe in nature. The quality of pain is sharp, dull and throbbing. The pain comes and goes and wakes him in his sleep. The patient is limping. Nothing has changed since the problem has started. Walking, standing, bending, squatting, kneeling, stairs and sitting make the symptoms worse.
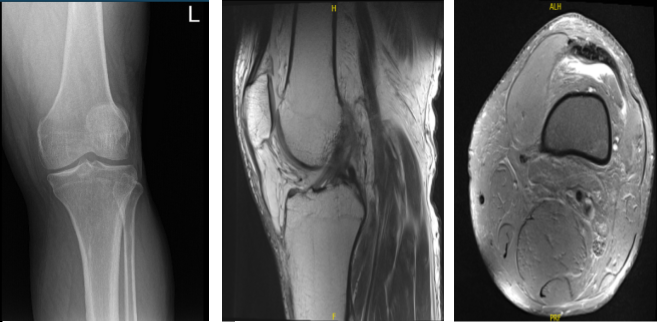
Xray presented no significant degenerative changes. Recommend a patient to take MRI. MRI results oblique flap tear in the posterior horn and body medial meniscus with associated para meniscal cyst measuring 8x3x3 mm.
Aside from this, it showed oblique tear in the body and posterior horn of the lateral meniscus. Also seen moderate knee joint effusion. Moderate bilateral popliteal cyst on C4. Focal chondral fissure in the lateral patellar facet.
X-ray Left Knee MRI-Left Knee
Discussed treatment options to patients, differences, risk and benefits between operative and cortisone injection. Patient decided to try cortisone injection and will return to the office when no improvement happens. After two weeks, the patient returned for physical therapy recommendation.
Six months later, the patient came back and mentioned that his knee did well until pain started worsening again. He is out of work which involves lifting, climbing and other activities that require strength of his knee. Aside from the pain, the patient also complained of popping sounds on his knee.
Patient opted for surgical treatment. The patient was seen in the holding area and we ultimately discussed multiple treatment options. We discussed risks and benefits and complications of surgical treatment including infection, bleeding, nonhealing, knee pain, exacerbation of arthritis, need for knee replacement, and repeat surgery in the future among others. We also discussed having the possibility of meniscus repair if it is repairable. The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating room table. General anesthesia was induced. Left lower extremity was prepped and draped aseptically in the usual fashion after putting it into a leg holder. The right lower extremity was put on a Versace pillow. Time-out was called. Preoperative antibiotic was given. Tourniquet was Inflated.
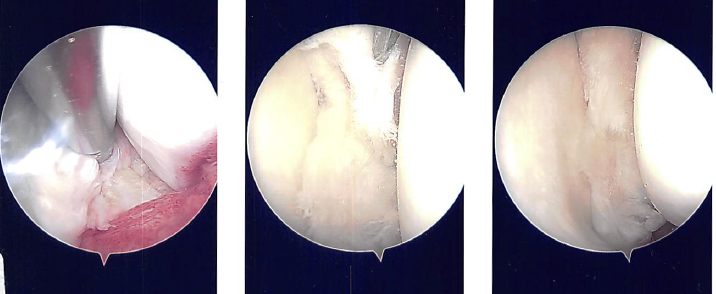
A lateral incision for the entry portal was created near the patella. The scope was given. The medial meniscus tear was visible after the scope was transferred from the patellofemoral joint to the medial compartment. The lateral compartment was examined with the scope, and it revealed fraying of the lateral meniscus and a tear in its anterior horn.
Making a medial entry portal with a spinal needle allowed for easier access to the medial and lateral compartments. A portal for entry was then created. Introduced to do the synovectomy was Shaver.
The complicated tear of the posterior horn and body of the medial meniscus was removed using upbitters and straight biters during the medial meniscectomy. Shaver was used to empty the parameniscal cyst and debride and transect margins.
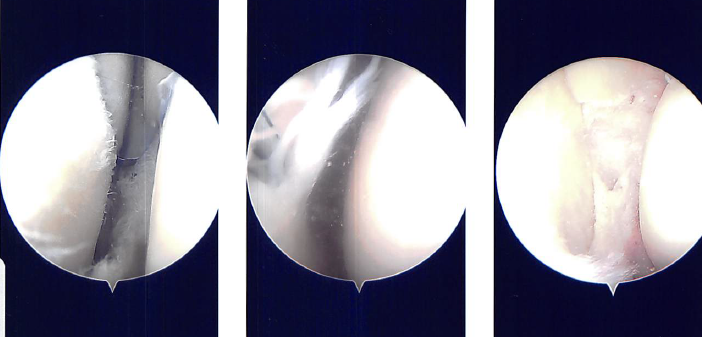
The knee was discovered to be intact when the scope was advanced to the intercondylar region. The lateral compartment received the scope. The anterior horn of the lateral meniscus was torn, and the medial edge of the lateral meniscus was frayed. The meniscus was cleaned off using a razor.
There were margins of balance. Final images were captured and stored. On the medial and lateral femoral condyles, there was no arthritis. There was grade 1 to grade 2 arthritis on the lateral tibial plateau.
The scope was moved to the patellofemoral joint where no arthritis was found over the patella as well as the trochlea. Final pictures were taken and saved. The knee was thoroughly lavage.
After a week of seeing patients, he has been improving with regards to pain and swelling. He is limping and has been using crutches for ambulation. Denies fever, chills, reinjury. After two weeks post-surgery the incisions are healing well, without evidence of drainage, erythema or warmth.
There is a full range of motion without discomfort. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.