Case Study: Knee Arthroscopic Lateral Meniscus
and Microfracture Chondroplasty
The knee is made to perform a variety of tasks, including supporting the body in an upright position without requiring the use of muscles. assists in raising and lowering the body. offers security.
An important stress absorber on the lateral surface of the knee joint is the lateral meniscus. That is the main reason why we need to pay attention fully to the knee conditions.
Patient is a 30 year-old male. Patient presents pain in his right knee and ankle. He is currently seeing a chiropractor treating him for his back. He also sees a neurologist for headaches. MRIs were reviewed and discussed.
MRI of his right knee was presented and clearly showed that there is tearing of the lateral meniscus anterior horn with parameniscal cyst tracking into the anterior intercondylar notch adjacent to the anterior root attachment site measuring 2 x 2.3 x 0.8 cm. Trace right knee joint effusion.
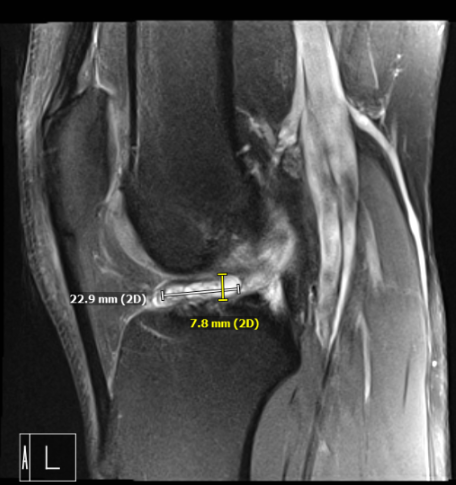
MRI of the right knee
We discussed treatment options and the patient opted for surgical management. We discussed meniscus repair versus meniscectomy. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, need for rehabilitation, possibility of failure and repeat surgery, systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was given. Antibiotics were given. The right lower extremity was prepped and draped aseptically in the usual fashion after application of tourniquet. It was put in a clamp. The left lower extremity was put on a well-padded pillow.
Arthroscopic set up was done and the time-out was called. A lateral entry portal was made and an arthroscope was inserted. The arthroscope was moved to the medial tibiofemoral compartment. A medial entry portal was made in a far medial position so as to reach the lateral meniscus easily. Shaver was introduced.
Examination of the medial compartment showed intact meniscus as well as chondral surfaces. Debridement of the intercondylar notch was done to remove the ligamentum patellae. The ACL was intact.
Examination of the lateral tibiofemoral compartment showed tear in the anterior horn as well as partial tear in the anterior root. The tear in the anterior horn was in the red-white zone and it was decided to repair it. Debridement of the anterior root of the lateral meniscus was performed.
The tear was prepped with the use of meniscal rasp and shaver. Outside-in repair was planned. Meniscal mender was opened and the straight needle was passed percutaneously laterally through the meniscus tear. The probe needle was advanced at the side of the straight needle through the tear.
Once it was in, the snare was passed out of the probe needle and PDS suture was passed through the straight needle The PDS suture was retrieved. A skin incision was given connecting the two sutures.
The PDS suture was replaced by #2-0 FiberWire. The repair was checked arthroscopically and found to be in a satisfactory position. The suture was knotted on the outside.
Examination of the rest of the lateral tibiofibular femoral compartment showed intact meniscus in the posterior horn as well as intact bone and cartilages. Examination of the patellofemoral compartment showed intact cartilage and no maltracking.
The final picture was taken and saved. The knee was thoroughly irrigated. To perform microfracture chondroplasty in the intercondylar notch to release the marrow into the knee to allow a good healing environment. Knee was drained completely.
Closure was done with #0 nylon. Dressing was done with the use of Xeroform, ABD, Webril, and Ace wrap. Knee immobilizer was applied. The patient was extubated and moved to recovery in a stable condition.
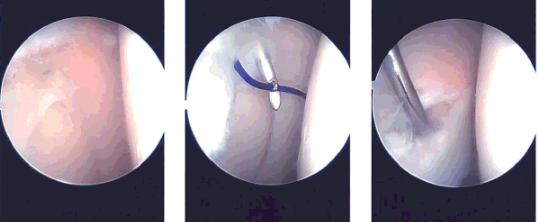
Intraoperative images
Patient requested to come back to the office with an MRI result. MRI impression as follows: Postsurgical changes of the lateral meniscus with mild recurrent tearing of the body segment and anterior horn however the appearance is improved compared to the presurgical study. Parameniscal cyst formation has resolved.
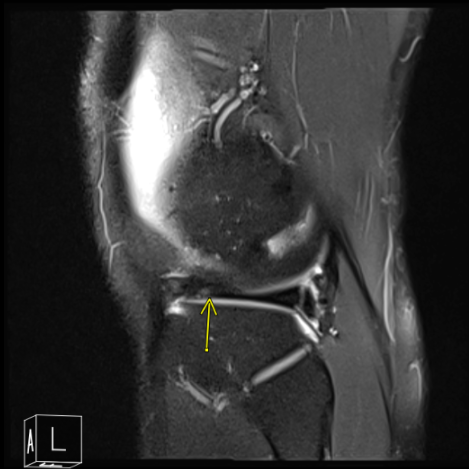
MRI of the right knee
He has been improving with regards to pain and swelling. He is limping and has been using crutches for ambulation. Denies fever, chills, reinjury. After two weeks post surgery the incisions are healing well, without evidence of drainage, erythema or warmth.
There is a full range of motion without discomfort. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
