Case Study: ORIF: Distal Radius Using Stryker Plate
and Screw with Distal Radioulnar Fixation using
Crossed Radioulnar K-Wire in a 63 year-old female
A modified Henry approach to the distal radius and a more ulnar approach, intended to expose the median nerve as well as the distal radius, are the two main palmar surgical methods to the distal radius. For the majority of distal radius fractures, the modified Henry method is appropriate.
The distal radius is the portion of the radius that connects to the wrist joint. Sometimes, a fracture in this region is referred to as a “broken wrist.” The most frequent causes of distal radius fractures are direct blows to the wrist or falling onto an outstretched hand.
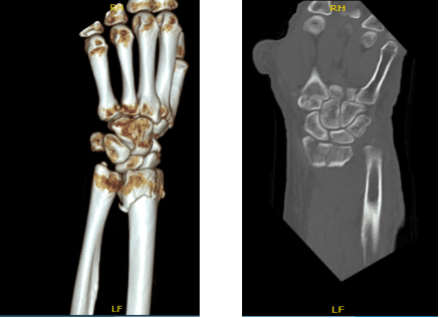
The patient is a 63 year-old female seen in the office with left wrist pain due to falling on the wrist. She was seen at Mather by Dr. Karkare where reduction was done. She got a CT done.
CT were reviewed and discussed by the doctor; there is a comminuted fracture of the distal radius with intra-articular extension where displacement measures approximately 1 mm. Maximal fracture displacement measures approximately 9 mm.
Approximately 20 degrees of palmar angulation are present. A displaced fracture of the ulnar styloid is also identified. Mild degenerative changes are present at the triscaphe and first carpometacarpal joints.
We discussed the treatment options and opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, nonhealing, need for repeat surgery, rehabilitation, systemic complications including blood clots, cardiac, pulmonary, and neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room, where she was placed on a well-padded operating table. General anesthesia was induced. Left upper extremity was prepped and draped aseptically in the usual fashion. Loban was used as a surgical site.
The fracture was checked under the fluoro and found to be displaced volarly. Incision was given over the flexor carpi radialis tendon. The anterior sheath of the flexor carpi radialis was cut in the line of the incision.
The tendon was retracted medially and the posterior sheath was cut. Pronator quadratus was reached, which was cut with the use of Bovie along the radial line. The fracture site was exposed. The fracture was comminuted and displaced.
With manipulation, the fracture was reduced and held with K-wire. The reduction plate was used and held with olive K-wires. This was found to move the fracture in good reduction. The plate was fixed to the proximal end using two cortical screws.
Pictures were taken and found that the fracture was well reduced. The fixation of the plate to the distal fragment was done with the use of the multiple locking screws. Two cortical screws were placed proximally. Final pictures were taken and found to be in satisfactory position. It was on the fracture site.
The fracture was thoroughly irrigated and packed with Vitoss. There was radioulnar subluxation. The wrist was put in supination and 1 to 1.5 mm K-wire was passed from the radius to the ulna and transfixing the distal radioulnar joint. Final pictures were taken and saved.
The wound was thoroughly irrigated and drained. Closure was done in layers using # 2-0 Vicryl and # 3-0 Monocryl. Dressing was done with the use of Xeroform, 4 x 8, Webril. Long arm posterior splint was applied. The patient was extubated and moved to the recovery room in stable condition.
The patient seen in the office for her postoperative visit with x-rays. She denies fever, chills and has poor pain tolerance and control. She is unable to move the fingers well and has swelling over the fingers and thumb.
X-rays were reviewed and discussed by the doctor; the patient is status post ORIF distal radius and ulnar styloid process fracture. Surgical hardware is in place in the distal radius. There is a fixation pin extending across the distal radius and ulna. The fracture fragments appear in satisfactory position and alignment.

Left wrist x-ray 2 views
After three weeks the patient was seen in the office for her postoperative visit with x-rays. She denies fever, chills, she has poor pain tolerance and control. Not able to move the fingers well and has swelling over the fingers and thumb and she was crying during the visit with any subtle movement.
X rays were reviewed and discussed. Good alignment and implant position Discussed treatment options including PT, MRI, Injection, surgery. We agreed to go with conservative management for now. Long arm splint and K wire removed.
Motivated for active and passive finger movement. Low threshold for pain. Has residual finger swelling with restriction of ROM Short arm splint applied due to poor pain control and OT to be started.

Left wrist x-ray 3 or more views
After two months the patient went to the office for her postoperative visit, she denied fever, chills. She has been working with OT and has been improving. Her finger swelling has decreased and she is able to move them more and She is weaning off the brace.
We decided the brace to be weaned off, motivated for active and passive finger movement and has residual finger swelling with restriction of ROM. OT to continue, Ice, Elevation and OTC anti-inflammatory meds. For follow up checkup the patient will be back after 4 weeks with x-rays.
After three months the patient is here today for her postoperative visit. She has no fever, chills, she has been working with OT and has been improving. Her finger swelling has decreased and she is able to move them more.
She has weaned off the brace and she is able to drive. X rays were reviewed and discussed. The fracture has healed. She is motivated for active and passive finger movement and has residual finger swelling with restriction of ROM.
And OT to continue, Elevation, OTC anti-inflammatory meds, follow up after 4 weeks and No X-rays needed. After the operation, the patient recovered well and kept up with physical therapy. The patient returned for a follow-up visit and her wrist had much improved.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
