Case Study: Meniscectomy, Chondroplasty
Patella fixation in a 35-year-old male
A patella fracture is a break in the little, flat bone that shields and covers the knee joint. Usually, a landing on your knee, a strike to the knee, or a collision due to an accident will result in a direct injury.
Having a patella fracture will frequently render you immobile and you may be unable to extend or lift your knee. Moreover, your knee’s range of motion, particularly its capacity to bend and extend, will be permanently lost.
It’s usually best to wait to try till you’ve been diagnosed if you think you can but it’s still uncomfortable. After receiving a patella fracture diagnosis and treatment, you will be permitted to bear weight while wearing a knee immobilizer, hinged knee brace, or cast that is locked in full extension.
A 35-year-old patient was in our office, with complaints of bilateral knees (left > right), back, and left shoulder pain. The patient remembers his injury in a motor vehicle accident.
The pain is moderate to severe in intensity and he described the pain as sharp, stabbing, and throbbing, which is constant and does disturb sleep. The problem has been getting worse since it started. Walking makes the symptoms worse but rest, heat, hot showers, and ibuprofen makes the symptoms better.
Patient stated he is currently taking psych medication at night before sleeping. Patient has no allergies and does not smoke. His left knee has been worsening. He has not been able to get a Miami J and knee brace.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line and has an effusion. The patient has discomfort with McMurray’s maneuvers, and the knee is stable.
They lack full flexion secondary to the effusion but have full extension. There is tenderness over the patella esp on the lateral half with a step off. There is also no erythema, warmth or skin lesions present.
A result for MRI was presented and shown mildly displaced patellar fracture with accompanying longitudinal tear of the distal quadriceps tendon. Bone contusion of the lateral femoral condyle. Large left knee joint effusion. Minimal undersurface fraying along the course of the medial meniscal posterior horn.
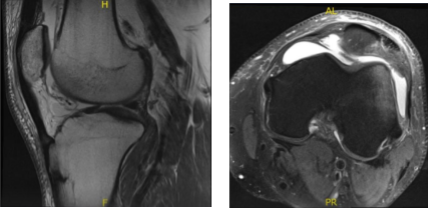
MRI – 3T Left Knee Non Contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands the risks of re-tear or failure to heal.
We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol. We discussed left knee arthroscopy and Patella fracture fixation vs excision left side and all indicated procedures.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. A high tourniquet was put on the left thigh. The lateral post was also kept for arthroscopy. The left lower extremity was prepped and draped aseptically. 3 g of Ancef was given prior to the surgery.
An Esmarch was applied, and tourniquet was raised to 325 mmHg. A lateral entry portal was made for the knee scope and the scope was entered. The patellofemoral joint was intact. The scope was moved to the medial compartment. Fraying of the medial meniscus was seen.
A medial entry portal was made using a spinal needle. The medial meniscus tear was excised using a straight biter and shaver. The scope was moved to the intercondylar notch where an ACL was intact. It was moved to the lateral femoral fraying of the medial margin of the lateral meniscus also.
The shaver and straight biters were used on the medial margin of lateral meniscus to a balanced margin. The scope was again moved to the patellofemoral joint where the fracture was seen and found to be displaced. The fracture was cleaned and an osteotome was used to release the fracture from the arthroscopic portal.
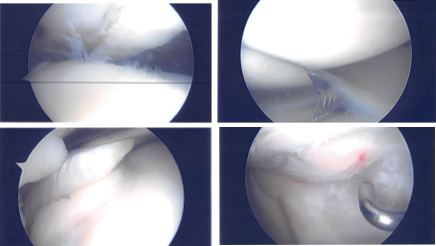
Intraoperative Arthroscopy Images
Now, the knee was put in extension and an anterior midline vertical incision was given to expose the fracture. With sharp dissection, the bone was reached. The lateral flap of the tendon was raised over the patella. The fracture site was reached which was mobile.
The fracture was reduced back and held with clamps. The two K-wires were passed. C-arm was introduced and checked and found to be acceptable reduction; 2 cannulated cancellous screws were inserted for fixation and compression.
The arthroscope was inserted to check the reduction and found to be appropriate. There was some cartilage damage around the edge which was debrided. Hemostasis was achieved. Closure was performed in layers after the closure of the quadriceps tendon and the paratenon.
The skin was closed using Monocryl. Dermabond and Steri-Strips were applied. Dressing was done. using Webril and Ace wrap. Knee immobilizer was applied. The patient was to be sent home with crutches and weight bearing as tolerated with antibiotics, aspirin, and pain medications.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We went over the arthroscopic pictures and removed the stitches during today’s visit.
We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatory and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. He will use Bledsoe knee brace and crutches (WBAT) for ambulation.
The patient was seen for post operative status post Left knee arthroscopic medial meniscectomy, lateral meniscectomy, chondroplasty, Open reduction, and internal fixation of fracture patella with arthroscopic assistance. He was using a knee immobilizer and crutches.
He had a small swelling on the upper most part of the incision which had decreased since the start of antibiotics. He had been doing well. He progressed to using a brace and ambulation FWB and doing PT with Block.
However, the patient was walking outside without a brace or walking aid when he slipped in some mud, heard a snap, felt sharp pain in the knee and collapsed to the ground. He was taken to Long Island Community Hospital where he had x-rays and was evaluated.
He is having pain from mid-thigh to proximal lower leg. The pain is continuous, and he is not sleeping. He is taking ibuprofen 800mg 4 times a day Percocet 5 mg.
A result for CT SCAN on Left knee was presented and shown comminuted displaced fracture of the patella with new fractures not seen on previous examination status post-surgery. Thickened appearance of the quadriceps tendon, there is excluded.
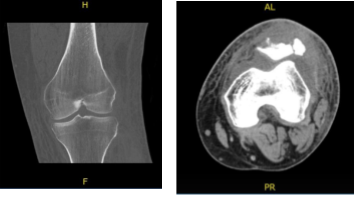
CT – Left Knee Contrast
Upon examination of the left knee reveals the incision is healing. The knee is slightly swollen and tender anteriorly. Range of motion 0-15 Quad set present. Normal alignment. Grossly normal stability.
There is no calf tenderness and a negative Homan’s sign. Sensation is intact to light touch distally and there is a brisk capillary refill. This is compared to the RLE which has more normal alignment, strength, stability and range of motion.
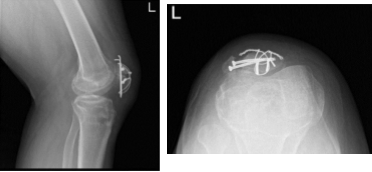
Left Knee X-ray Complete with Patella
Patient checked in for a follow up visit after a month and saw significant improvement on his knee. Results for the X-ray were presented and showed revision of the fractured patella with no instrumentations.
Since prior examination noted the presence of a 1.4 cm cystic lesion in the anterior aspect of the medial patella, dislocation has been developed since prior examination.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

