Knee Meniscus
If knee pain becomes more severe, disrupts daily activities, or is accompanied by swelling and redness, it is important to see a healthcare provider. At Complete Orthopedics, our skilled team specializes in managing knee meniscus tears with personalized treatments and surgical options. We focus on understanding your symptoms, identifying the root causes, and suggesting the most appropriate treatments or surgical interventions.
Our facilities are located throughout New York City and Long Island, with affiliations to six leading hospitals, ensuring access to high-quality care for knee problems. Schedule an appointment with one of our orthopedic surgeons online or by phone. Discover the causes and treatments for knee pain, and determine when surgery might be necessary.
Overview
Anatomy
The knee joint is a very complex joint, which is made by the lower end of the thigh bone or the femur on the top and the upper end of the shin bone or the tibia below. It also has knee cap or the patella in front, which essentially moves in a groove over the front of the lower end of the thigh bone called trochlea. The lower end of the thigh bone and the upper end of the shin bone articulate with each other in two compartments, the inner or the medial compartment and the outer or the lateral compartment.
The two compartments have a fibrocartilaginous disk in between the two articulating surfaces each. These C-shaped articulating fibrocartilaginous disks are called the meniscus (plural – menisci).
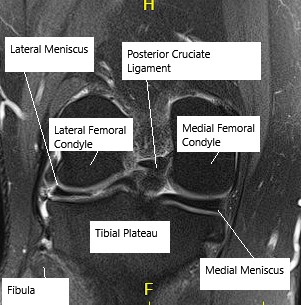
MRI showing knee meniscus.
The meniscus helps in smooth movement of the knee, which includes flexion and extension, gliding as well as rotation. They act as shock absorbers and helps in spread of the forces of the joint over a wider surface area and hence decreasing the pressure and preventing damage to the articular surface.
These menisci are attached from the outer side to the joint capsule from where they also received their blood supply and the nutrition.
There is no blood supply to the meniscus from inside the joint. Hence, the blood supply of the meniscus is richest to the outer most part of the meniscus and decreases gradually as it goes towards the inside of the joint so much so that there is almost no blood supply to the inner most part of the meniscus.
This peculiar characteristic is important in understanding the pathology and their management. Medial meniscus is the commonest meniscus of the two to be torn. Medial Meniscus is less mobile because it is attached firmly to the inside of the joint capsule and the deep part of the medial collateral ligament.
Pathology
The meniscus as every other part of the body also ages as we grow older, the process being called degeneration. The process of degeneration may be accelerated due to knee injuries which may or may not be recalled for; in the form of one specific trauma or multiple micro injuries.
Contact sports may be a factor in early degeneration of the meniscus and of the joint. Meniscus are usually injured due to twisting force over the knee in which the meniscus is caught between the two articulating surfaces and gets ripped to form a tear. Meniscus is more prone to a tear if it is degenerative.
A meniscus injury can occur in isolation or may be a part of multiple injuries to the knee, which may include ligamentous injury especially the anterior cruciate ligament, medial collateral ligament or injury to the cartilage of the knee. Occasionally, meniscal tear may be found with stress fracture or bone marrow lesion or bone marrow edema of the adjacent bone.
Meniscal tear in young population is mostly caused due to sporting activity or an accident. Meniscal tear in elderly population can be caused due to microtrauma or injury, which may or may not be recalled. There are multiple types of meniscus tear like horizontal, vertical, radial, bucket handle and complex.
The bucket handle tear is usually found in younger population. The meniscal tear usually involves one of the two menisci, the most common being medial meniscus.
Symptoms
Symptoms of a meniscal tear include:
- Pain in the knee
- Swelling
- Stiffness
- Difficulty straightening the knee
- Feeling of the knee giving way or locking
A meniscal tear may present with a sudden onset of pain and swelling after an injury or fall. The swelling usually occurs over a period of few hours or may be overnight.
An audible click or pop may be heard at the time of injury. It may also present with feeling of giving way or an episode of locking in which the knee is stuck in a specific position and may or may not get free by maneuvering it out of it. The patient may also have limp due to pain and may need the help of cane or crutches to ambulate.
In patients with degenerative meniscus, the presentation may be subtle, in the form of pain and recurrent effusions or swelling of the knee, which may subside over time only to recur. These patients usually have a point tenderness to touch in the area of the tear.
Diagnosis
The physical examination done by the physician may be suggestive of a tear. The physician also examines for other injuries of the knee including the ligamentous injury. X-rays of the knee on the first line of investigation and they are done to rule out any fractures or subluxations of the knee. MRI is confirmatory investigation and the investigation of choice to confirm a meniscal tear.
The MRI also helps to know the configuration of the tear, which in turn helps in planning of the treatment.
Types of Tears
Meniscal tears are classified by their location and pattern:
- Horizontal Tears: Parallel to the tibial plateau.
- Longitudinal (Vertical) Tears: Perpendicular to the tibial plateau.
- Radial Tears: Perpendicular to both the tibial plateau and the long axis of the meniscus.
- Complex Tears: Combination of different types.
- Displaced Tears: Detachment or flipping of a meniscus piece.
Treatment of a meniscal tear in presence of arthritis
Meniscal tear under degenerative setting can be initially treated conservatively with the use of antiinflammatory medications, elevation, icing, compression, use of physical therapy with or without the use of cortisone shot.
These all help in decreasing the inflammation and the swelling of the knee and helping in returning the function of the knee to normal. If the patient does not have relief from all these conservative measures or there is recurrence of the symptoms, then an MRI can be done to confirm diagnosis and a surgical treatment in the form of arthroscopic management of the meniscus can be done.
Treatment of meniscal tear in the younger population
Younger population usually presents with acute presentation of the meniscal tear. An MRI is usually performed in these patients to confirm the diagnosis as well as rule out other injuries to the knee. It is always advisable to keep the native meniscus in place especially in younger population because meniscectomy has been shown to enhance or accelerate the osteoarthritic changes in the knee in the future.
If the meniscal tear is repairable, it should be repaired with the use of sutures on the meniscus. This was usually performed arthroscopically and should be done as soon as possible to improve the chance of healing and full recovery. If the meniscus is non-repairable then a partial meniscectomy has to be performed to debride the meniscus and remove the loose flaps which are contributory to the pain, catching sensation and swelling in the knee.
Surgical treatment
Patients are usually called on the day of surgery and operated arthroscopically. Post surgery, patients are discharged to home in a couple of hours with prescription for pain medications, along with brace and crutches if needed. Patients who undergo meniscal repair are usually given a femoral block, which will make their leg weak for about 24 hours.
They are also provided with the ice pack to control their pain and swelling. All patients are encouraged to use ice, elevation for one week after the surgery or more if the pain and swelling persist. Patients can take off their dressing in 72 hours and shower keeping the dressing dry.
Post-meniscal surgery rehabilitation
The patients are usually seen one week after the surgery. Patients who have undergone meniscectomy do not need the use of brace and are put in physical therapy to improve their movements, range of motion as well as strength in their muscles. It may take 3 to 6 weeks to recover from the surgery.
These patients usually do not have any limitation with regards to their movement and can perform activities of daily living within the limits of toleration of pain.
They are usually allowed advance activities by 6 to 10 weeks after surgery. The patients who undergo meniscal repair do need to be in a knee brace. They are usually allowed to bear partial weight on the operated extremity with the brace locked in extension and the help of axillary crutches for ambulation.
They are seen one week after the surgery and physical therapy is initiated. They are allowed to move their knee through range of motion without weightbearing. They are encouraged to strengthen their muscles as well as improve their range of motion.
Range of motion and weightbearing is usually allowed at 6 to 8 weeks post surgery when the brace has gradually weaned off. The patients are not allowed to participate in contact sports for about 3 to 4 months after the surgery.
Prevention
To prevent meniscal tears:
- Strengthen leg muscles, especially the quadriceps.
- Warm-up before exercising.
- Avoid activities that involve sudden twists and turns.
Complications
- Infection
- Bleeding
- Nerve or vessel Injury
- Failure of repair to heal
- Hemarthrosis
Do you have more questions?
What is the function of the meniscus in the knee?
The meniscus acts as a shock absorber, distributes weight, provides joint stability, and aids in smooth knee movement.
How can I differentiate between a meniscal tear and other knee injuries?
Meniscal tears often present with specific symptoms like knee locking, inability to fully straighten the knee, and pain localized to the joint line. Diagnosis usually involves physical exams and MRI.
How effective are conservative treatments for meniscal tears?
Conservative treatments like RICE, physical therapy, and NSAIDs can be effective, especially for minor or degenerative tears.
When is surgery necessary for a meniscal tear?
Surgery is necessary when the tear is large, symptomatic, or unresponsive to conservative treatments, and particularly if the tear is in the red zone, which has better healing potential.
What types of surgical procedures are available for meniscal tears?
Surgical options include meniscectomy (removal of the damaged part) and meniscal repair (suturing the tear).
What are the risks associated with meniscal surgery?
Risks include infection, stiffness, continued pain, and potential for accelerated arthritis if the meniscus is removed.
How long does recovery take after meniscal surgery?
Recovery varies but typically takes several weeks to months. Full rehabilitation includes physical therapy to restore strength and mobility.
Can meniscal tears heal on their own without surgery?
Some tears, especially those in the red zone with a good blood supply, can heal with rest and conservative management.
What activities should be avoided with a meniscal tear?
Activities involving twisting, squatting, or heavy lifting should be avoided to prevent further damage.
How can I prevent meniscal tears?
Strengthening leg muscles, proper warm-up exercises, and avoiding sudden twists can help prevent tears.
What is the prognosis for a meniscal tear?
The prognosis depends on the tear’s location, size, and treatment method. Many people recover well with appropriate treatment.
Are there any long-term complications of untreated meniscal tears?
Untreated tears can lead to chronic pain, knee instability, and increased risk of developing osteoarthritis.
How does age affect meniscal tear treatment and recovery?
Older adults may have more degenerative tears and slower healing, often requiring a more conservative approach or surgery based on overall health.
Can physical therapy alone heal a meniscal tear?
Physical therapy can strengthen surrounding muscles and improve function, potentially aiding in the healing of minor tears.
What are the signs of a meniscal tear in athletes?
Athletes may experience knee pain, swelling, popping sensations, and difficulty moving the knee.
How common are meniscal tears?
Meniscal tears are common, especially among athletes and older adults due to injury and degenerative changes.
What is the difference between a partial and complete meniscectomy?
A partial meniscectomy removes only the damaged portion, while a complete meniscectomy removes the entire meniscus, which is rare due to high risk of arthritis.
Can meniscal tears occur alongside other knee injuries?
Yes, they often occur with ligament injuries like ACL tears.
What role does imaging play in diagnosing meniscal tears?
MRI is the most accurate imaging tool for diagnosing the type and extent of meniscal tears.
Can diet and supplements aid in meniscus healing?
A balanced diet rich in anti-inflammatory foods and supplements like glucosamine may support joint health, though evidence is mixed.
What are the potential complications of meniscal repair surgery?
Complications can include infection, blood clots, and the possibility that the repair doesn’t heal properly, necessitating further surgery.
How does weight affect meniscal tear risk and recovery?
Excess weight increases stress on the knee, raising the risk of tears and complicating recovery.
Are meniscal tears more common in certain sports?
Sports that involve a lot of twisting and pivoting, like soccer, basketball, and skiing, see higher rates of meniscal tears.
What is the likelihood of re-tearing the meniscus after surgery?
Re-tear risk depends on factors like the tear type, repair quality, and post-surgery care but can occur, especially if the knee is subjected to high stress too soon.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
