Case Study: Knee Arthroscopic: Lateral Meniscectomy
and Chondroplasty in a 47-year-old female
Meniscectomy is a common orthopedic procedure used to relieve knee pain in the elderly population with meniscal pathology; it is typically carried out on older patients with degenerative meniscal tears. Arthroscopic chondroplasty is a common surgical procedure carried out during knee arthroscopy; it is specifically used to smooth damaged cartilage in the knee to lessen friction in the joint.
A 47 year-old female patient was seen by a doctor in the office multiple times after her accident. we did a surgery on her right shoulder, which has recovered uneventfully. She has been complaining of pain in her right knee since the accident.
An MRI was done, which showed an osteochondral lesion in the patellofemoral joint. She had no relief with nonoperative treatment. We discussed treatment options and operative surgical management.
We discussed risks and complications and benefits including infection, bleeding, injury to the adjacent nerves and vessels, failure of surgery, need for repeat surgery, development of arthritis, and need for total knee replacement in future among others.
We discussed systemic complications including blood clots, cardiac and pulmonary complications among others. The patient understood and signed an informed consent.
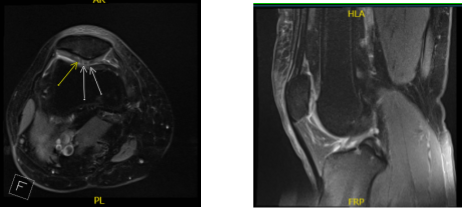
MRI Right knee non-contrast
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. The right lower extremity was prepped and draped aseptically in the usual fashion. The tourniquet was elevated. A time-out was called.
Preoperative antibiotic was given. A lateral entry portal was made and an arthroscope was inserted. Examination showed grade 2 to grade 3 osteochondral lesions over the posterior surface of the patella. A medial entry portal was made with the use of a spinal needle.
Examination of the medial tibiofemoral compartment showed intact medial meniscus and cartilage. Examination of the intercondylar notch showed intact ACL and PCL.
Examination of the lateral tibiofemoral compartment showed intact cartilage, but there was fraying of the anterior horn of the lateral meniscus, which was debrided with the use of a shaver to perform a lateral meniscectomy.
A shaver was also used to debride the posterior surface of the patella. Final pictures were taken and saved. The knee was thoroughly irrigated and drained. Closure was done with 3-0 nylon.
Then, 30 mL of 0.5% Marcaine mixed with 40 mg of Depo-Medrol was injected into the knee. The dressing was done with the use of Adaptic, 4×4, ABD, Webril and Ace wrap. The patient was extubated and moved to Recovery in a stable condition.
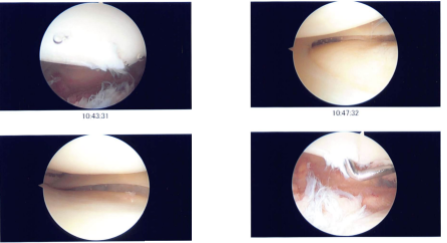
Intraoperative photo
She is here for her postoperative visit. She removed the sutures by herself at home. She denies fever, chills and pain has improved. She is back to work and she plans to do PT by herself. Discussed treatment options including PT, MRI, Injection, surgery.
We agreed to go with conservative management for now. PT to be started as discussed. With regular visits in the office, the patient did well after the surgery and continued physical therapy for the knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.