Osteoarthritis is the most common form of arthritis affecting middle-aged to elderly patients. Commonly known as the joints’ wear and tear arthritis, osteoarthritis involves all the structure forming the synovial joint rather than just the cartilage at the ends of the joint. Osteoarthritis is a progressively deteriorating condition that is usually managed with joint replacement surgery in advanced cases.
A joint is formed where the ends of two bones meet. The bone ends are covered by protective cartilage known as articular cartilage, a tough glistening smooth tissue. A joint capsule encases the joint, which also secretes synovial fluid.
Synovial fluid lubricates the joint and provides nutrition to the articular cartilage. Various ligaments support the joint, which provides stability. Different groups of muscles cross the joint, and their coordinated stimulus results in movement of the joint.
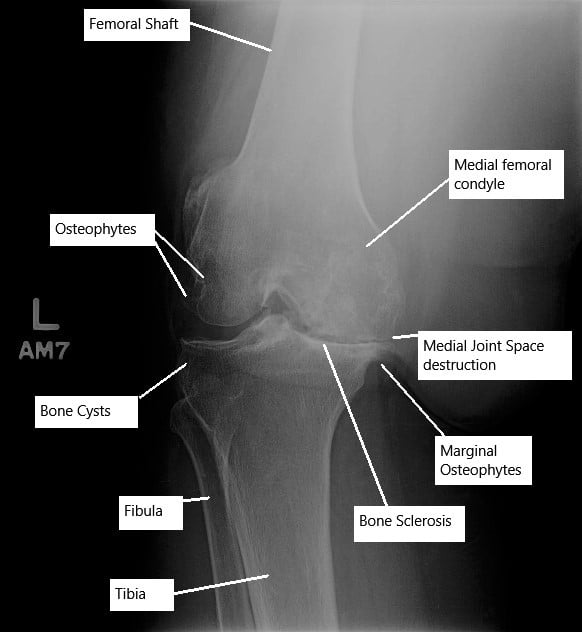
Advance osteoarthritis of the left knee joint on an X-ray.
In the disease process of osteoarthritis, the articular cartilage erodes which results in constant grinding as the joint moves. Primary osteoarthritis of any joint arises without any known underlying disorder.
It tends to occur more frequently after the age of 50 and is more common among women. Obesity has been implicated as a cause of primary osteoarthritis.
Secondary osteoarthritis results from any disease or injury which damages the structures forming the joint. Various causes have been implicated in secondary osteoarthritis.
Secondary arthritis may result from rheumatoid arthritis, malalignment of joints, tendon or ligament injuries, gout, diabetes mellitus, intra articular bleeding in hemophilia, acromegaly, Injuries to the cartilage, etc.
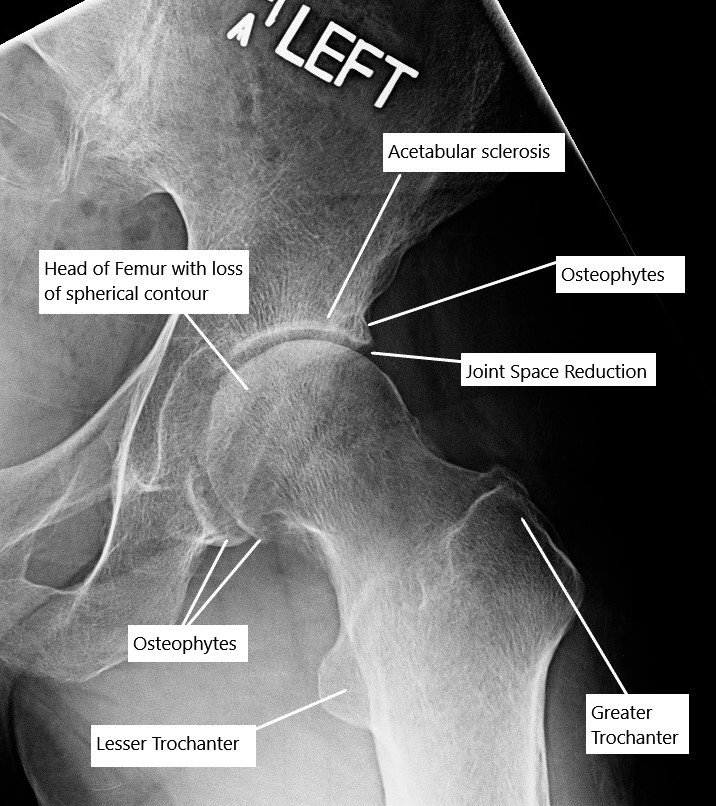
Osteoarthritis of the hip joint on an X-ray.
In the early stage of osteoarthritis, there is swelling of the articular cartilage, there is the appearance of fissures and cracks in the articular cartilage. The body attempts to repair it by increasing blood supply with the formation of new blood vessels. The new blood vessels invade the subchondral bone which leads to its increased density.
The destruction of the cartilage continues leading to decreased joint space visible on radiographs of large joints. The degenerated cartilage either dissolves in the joint or forms ‘’loose bodies’’ inside the joint. T
he body tries to repair the exposed bone resulting from the denuded cartilage. The repair leads to thickening and overgrowth of the subchondral bone. The thickening of the subchondral bone is especially prominent at the sides of the joint which appear as bone spurs.
The synovial membrane of the joint undergoes hyperplasia, which is swollen and inflamed. There is a development of cysts/cavities in the subchondral bone at the places of maximum stress. The pressure inside the joint increases as a result of decreased venous outflow and an increased arterial flow in the subchondral region. The increased pressure leads to the symptoms of pain at rest.
Osteoarthritis may involve multiple joints but is most common in the hands, knees, hips, and shoulders. The disease is progressive, but the symptoms are usually not consistent.
There may be a flare-up of the symptoms, and at other times, they may come and go. The most common symptom is pain, which is usually worse at the end of the day, and the intensity and frequency of pain increases as the disease progresses.
The patients may describe the pain as a sharp or dull pain located in the joint or at the joint’s sides. The joint pain typically gets worse with activity involving the joint. As the disease progresses, the pain may be associated with swelling of the joint.
The patients also complain of the grinding sound known as crepitus on moving the joint. There may be episodes of locking of the joint due to the loose bodies’ impingement, especially in the knee joint.
There is an associated stiffness of the joint, which is worse after prolonged periods of inactivity. The stiffness is usually worse in the morning. Patients associate changes in weather with joint pain. The pain is generally worse in cold weather when the barometric pressure drops outside the joint, leading to increased swelling inside the joint.
As the disease progresses, there is a gradual restriction of joint movement. The muscles around the joint also become weak and frail secondary to decreased motion.
The diagnosis of osteoarthritis is made based on history, physical examination, and radiological evidence. A detailed history regarding the onset of symptoms and associations is taken, which is followed by a physical examination of the involved joints. Blood investigations may be done to rule out systemic diseases such as rheumatoid arthritis, gout, or any infection.
Plain radiographs are usually the first radiological test done to look for joint space reduction, cysts, and thickening bones. In some cases, for a detailed evaluation, a CT scan or an MRI may be ordered. An MRI gives the details of all the soft tissue structures inside the joint, which are not visible on an X-ray.
In some cases, joint aspiration or arthrocentesis may be done, which involves taking a tiny amount of synovial fluid from the joint using a syringe. The contents of synovial fluid are then subjected to lab tests.
The management of osteoarthritis depends on the severity of the disease and the lifestyle limitation as a result of the disease. Non-surgical treatment forms the first line of management that involves weight loss, physical therapy, cold and heat therapy, and nonsteroidal anti-inflammatory medications.
Intra-articular steroid injections may be administered in the joint by the surgeon. Intra Articular steroid injections decrease the inflammation associated with osteoarthritis. Significant pain relief is obtained, but the effects wear off after a few months.
Repeat injections may be needed. Certain medications such as glucosamine, chondroitin sulfate, diacerein, and hyaluronic acid have been used, but controversies surround their actual benefit.
The surgical management may involve procedures such as arthroscopic debridement of the joint in the early stages of osteoarthritis. Arthroscopic debridement involves the use of a keyhole incision through which a tiny camera is inserted along with instruments. All the dead tissues and loose bodies are removed.
In large joints such as the knee joint, bone-cutting surgery known as osteotomy may be done to change the alignment of the forces acting on the joint. It decreases the pressure on the area of the cartilage involved in osteoarthritis, but it is only helpful in the early stages of the disease.
Osteoarthritis is a progressive disease that continues to progress despite interventions, and ultimately most patients may require joint replacement surgery. Joint replacement surgery has revolutionized the management of osteoarthritis. The joint ends are replaced or resurfaced with metal and plastic parts.
The prosthetic parts recreate the joint movements. The alignment of the joint line is created as it was before the disease process. Joint replacement provides a pain-free joint with a near-normal range of motion. Recent advances have ensured that most artificial joints last 15-20 years or more.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
