Case Study: Meniscectomy and Patellofemoral
Chondroplasty in a 60-year-old Female
The patient is a 60-yr-old female, with complaints of left knee pain. She does not recall any injury. She first experienced the pain last year while walking and the pain has worsened since it began. The pain is extremely severe in intensity (8/10). The patient describes the pain as sharp and on the inside of the knee. The pain is constant and does disturb her sleep.
The pain is associated with mild swelling. The problem has been getting worse since it started. Walking and standing make the symptoms worse. Rest makes the symptoms better. The Patient has not undergone any surgery in the past. Her medical history is positive for diabetes and hypertension both under control with medications. She is a school teacher with much of her working hours spent standing. She denies any known drug allergies. The patient is a nonsmoker and social drinker.
The patient is calm, conscious, cooperative and well oriented to time, place and person. On examination of the left knee, the patient is tender to palpation along the medial joint line and has an effusion. The patient also has patellofemoral crepitus and there is tenderness on palpation along the medial and lateral patellofemoral joint line. The patellar grinding test is positive.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable on anterior, posterior, medial, and lateral stress tests. The left knee lacks full flexion secondary to the effusion but has a full extension. The left knee has 5/5 strength and is neurovascularly intact distally. There are no erythema, warmth, or skin lesions present.
On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.

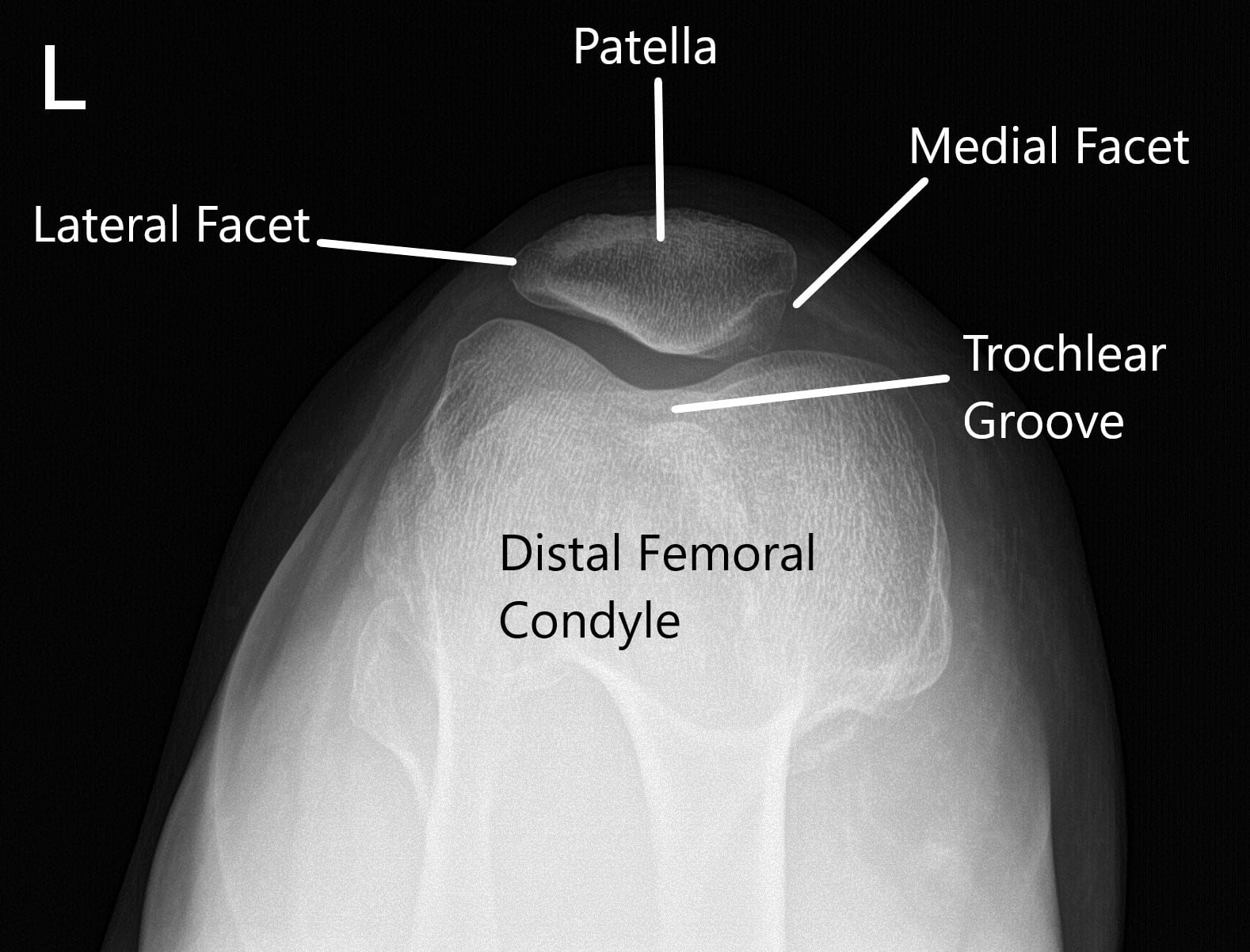
X-ray of the left knee in AP and skyline view of the patella.
MRI of the left knee suggested a medial meniscal tear and medial and patellofemoral compartment articular cartilage defects.

We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits. The patient has expressed a desire to proceed with the surgery. Risks, benefits, alternatives, and postoperative protocols were discussed with the patient at length.
Under anaesthesia and aseptic cleaning and draping, a lateral working portal was then established in the left knee and the knee scope was entered. Examination of the knee showed patellofemoral arthritis, especially in the distal medial patellar facet.
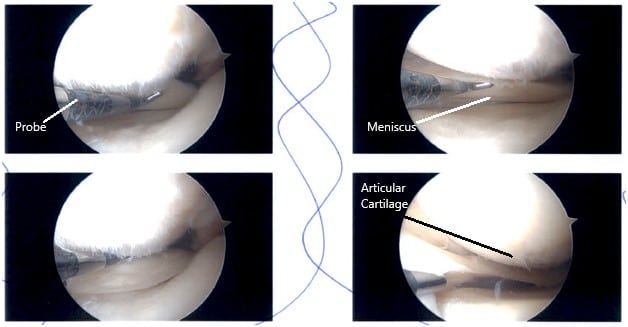
Intraoperative Arthroscopy images.
There was an inner free margin tear on the medial and lateral meniscus. An undersurface softening of the posterior horn of the medial meniscus was identified with no open lesion.
The ACL was intact in the intercondylar notch. The cartilage of medial and lateral femoral condyle was intact. There were grade 1 to 2 changes in the trochlea and grade 3 to grade 4 changes in the medial inferior patellar facet. The inner margin of the medial and lateral meniscus was balanced through a stable margin.
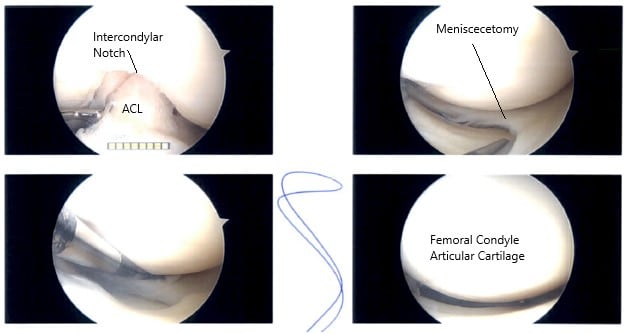
Intraoperative Arthroscopy images.
The knee was reexamined again. Arthroscopic pictures were taken. Chondroplasty of the inferomedial patellar facet was performed and pictures were taken. Partial synovectomy of the the medial femoral gutter was performed.
The knee was irrigated and washed thoroughly. Closure of the knee was performed using nylon #3-0. Dry dressing with Adaptic, 4 x 4, and Webril was performed. Thigh-high TED hose was applied. The tourniquet was removed. The patient was extubated and moved to the postoperative recovery unit in a stable condition.
Patient did well after the surgery and physical therapy was started in 1 week. She had a good result and was able to get back to usual activities in 4 weeks.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
