Knee Cartilage Injuries & Management
If knee pain becomes severe enough to disrupt daily activities or is accompanied by swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our expert knee doctors specialize in treating knee pain using both non-surgical and surgical methods. We evaluate symptoms, diagnose the problem, and suggest suitable treatment options, including surgery when necessary.
We operate in New York City and Long Island and are associated with six hospitals, offering advanced knee surgery and comprehensive orthopedic care. You can book an appointment with our orthopedic surgeons online or by phone.
Discover the typical causes of knee pain and the treatments available, including when surgery is the most advisable course of action.
Overview
Cartilage is a glistening white smooth tissue covering the ends of bones where it articulates with other bone and form a joint. It is toughened yet flexible enough to cushion the gliding of the bones forming the joint. Knee is a large weight bearing joint with forces up to 8 times body weight passing through it with every step.
Articular Cartilage helps in reducing friction by acting as a slippery cushion and a shock absorber. This allows for smooth movements of the knee joint.
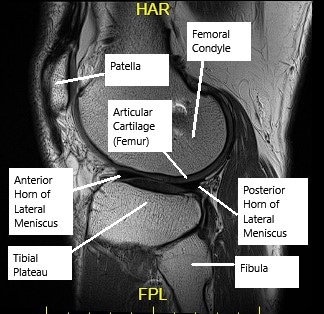
MRI of the knee showing articular cartilage.
Apart from the above mentioned unique properties it has a limited blood supply so any damage to the cartilage will not heal optimally on its own.
The most common form of cartilage damage is age related degeneration or wear and tear of the joint known as osteoarthritis.
Contrary to the age related degeneration, primary injuries to the articular cartilage usually occur in young and active population. It can lead to early deterioration of joint causing secondary osteoarthritis.
Symptoms
- Knee Pain: Damage to the articular cartilage of knee occurring in an otherwise healthy patient presents most commonly with knee joint pain.
- Swelling and Stiffness: The pain is usually associated with swelling, knee effusion and stiffness, especially worse during walking, jogging or sports activities.
- Feeling of Knee Giving Away: Patients may also experience symptoms of their knee giving away, catching, instability or may have a grinding sensation in the knee during day to day activities.
- Locking: Sometimes the cartilage breaks from the bony end and comes to lie freely in the joint known as a ‘loose body’. This loose body might cause episodes of locking of knee. The patient might not be able to extend (straighten) or bend their leg from a particular position.
These are all symptoms that slowly deteriorate over time, causing a significant morbidity in day to day activities. Young athletes may find themselves off field and may affect their career. Over time the condition may lead to degenerative changes secondary to the cartilage injury and altering of the normal biomechanics of the joint.
Causes
- Trauma/Injuries: The condition is particularly common among athletes and active adults engaging in sports. Here the injury is usually a result of the direct impact on the articular cartilage which may be small or large in size with a varying amount of depth of lesion. Lesions reaching the bone lying directly under the cartilage (called subchondral bone) are a result of significant trauma.
- Overuse: Other common cause is repetitive overuse of the joint in active adult population leading to microfractures of the underlying bone and cartilage which progresses to a full depth cartilage injury.
- Congenital(since birth): Some people with abnormalities of the joint by birth are predisposed to the cartilage injury as abnormal forces act on certain areas of the knee which would be otherwise distributed in a normal adult. Such individuals have altered biomechanics of the knee.
- Osteochondritis dissecans: Conditions such as Osteochondritis dissecans occur more frequently in children. Here the underlying bone loses its vascularity or blood flow. The bone upon losing the blood supply slowly dies or gets degraded. The body tries to form new bone and replace the dead bone but in the process the overlying piece of cartilage is damaged.
Certain endocrine/hormonal abnormalities, vascular diseases, unknown causes or simply hereditary factors predispose to the development of osteochondritis dissecans.
Diagnosis
- History & Examination:Physician will take a detailed history preceding your condition and any injuries or surgeries around the knee. They will conduct a thorough physical examination including clinical tests and measurements to check for instability.
- X-Ray/CT Scan: Usually a radiograph/X-ray is the first investigation done to check for bony integrity ruling out fractures which can be further aided with a superior CT scan.
- MRI: For cartilage injuries the best investigation is an MRI which can provide a detailed view of all the sectors of the cartilage and any damage to the surrounding ligaments and knee pads (meniscus) which stabilize the knee.
- Diagnostic Arthroscopy: Arthroscopy when used for diagnosis is the gold standard. Here a tiny camera is inserted through a keyhole providing a telescopic view of the entire knee joint. Treatment of the condition can also be done at the same time using arthroscopic instruments.
Treatment
Treatment depends on a number of factors like age of the patient, the size of defect,demands of the patient and ability to tolerate rehabilitation.
Nonsurgical Treatment
Nonoperative treatment usually consists of anti-inflammatory medications, physical therapy and braces to unload the injured cartilage. Some other options like steroid injections or viscosupplementation are controversial especially in young patients. All conservative options focus on relieving the pain and giving time for the cartilage to repair itself. But the defect rarely heals on its own and generally progresses over time.
Surgical Treatment
Surgical techniques can be compared to filling a pothole and options involve either the use of minimally invasive Arthroscopic technique or invasive open procedures called arthrotomy.
Generally arthroscopic surgeries provide earlier return to previous activity and lesser hospitalization. Most of them are day care procedures. Arthroscopic surgery utilizes 2-4 keyhole incisions through which a mini camera is inserted providing a telescopic view and fine pencil size instruments are inserted to do surgical procedure.
Debridement / Chondroplasty
In this surgery, usually performed with an arthroscope, the friable cartilage is simply removed and cleaned. Although it promises a very fast rehabilitation and recovery but success rates are variable and is successful in very small and superficial defects. The cleaned up area is filled with a tissue by the body but this tissue is not as good as the original cartilage itself.
Microfracture Technique
Several small micro-holes are created in the underlying bone through keyhole surgical techniques like arthroscope. Multiple drills cause marrow bleeding in the defect thereby allowing cells with regeneration potential to fill the defect and over time these cells form the new cartilage tissue.The technique is quite effective in small defects and is cost effective being a single stage procedure. But it requires the patients to remain non weight bearing for a long period of time.
Mosaicplasty
It involves filling of the defect from patients own cartilage as a graft taken from a non weight bearing portion. The defects are filled and the body’s own grafted cartilage incorporates into the defect along with bone plugs. The procedure can be done for small full thickness defects in weight bearing area and require the availability of normal cartilage for grafting.
This technique avoids the problems of graft rejection and high costs. The non weight bearing areas of the cartilage are accessed through keyhole surgery using arthroscopy and matched to shape exactly the size of the defect. Rehabilitation is expedited and offers good results. As there are multiple grafts planted in the defects hence looking like mosaic. The surgery is usually day-care and patients usually return to their previous activities after a period of physical therapy.
Allograft Osteochondral Transplantation
The bone and cartilage graft is taken from a cadaver i.e preserved cartilage and bones from a dead donor. The graft is matched and shaped to fill the defect. The graft is especially prepared and processed to prevent transfer of infections.
This is useful in patients with larger defects in young patients. It is done through open technique. A right size graft is shaped to exactly match the defect and fixed. The grafted cartilage is incorporated in the defect with time and the patient can then resume his daily activities.
Fixation of fragments
In case of children and young patients, especially those suffering from osteochondritis dissecans, a large fragment can be simply fixed back to the underlying bone with sutures or screws. Helpful in fresh cases when the cartilage fragment is usually hanging by a tissue in the joint.
This helps in retaining the patient’s anatomy and native bone and cartilage. The sutures and screw fixation can be done using arthroscopy technique which not only treats but helps to detect any other cartilage problems within the knee as the whole joint is inspected using the telescopic camera.
Autologous Chondrocyte Implantation
In this two step surgery usually spanning several weeks the patient’s own cartilage cells are first harvested from the non weight bearing areas of the joint and then grown in a special medium in the lab. Over the course of several weeks the cells multiply and they are then placed in the defect of the cartilage which is covered by periosteum (covering of the bones).
The cells have regeneration potential meaning they can form the native cartilage when placed in the defect. The surgery is usually performed using an open technique in which the knee joint is opened and the area is directly accessed. Rehabilitation takes several weeks and the patient can then resume his activities.
Knee replacement
Reserved for older age group with chronic cartilage damage leading to osteoarthritis changes. Here the joint surfaces are replaced with prosthetic material to re-create the normal motion of the knee. The joint is divided into two compartments one on the inner side and the other on the outer side. The inner side is more frequently involved and in patients with a normal outer side and undergo a semi knee transplant called Unicondylar knee arthroplasty using a minimally invasive technique. It offers an expedited rehabilitation and resumption of activities.
In patients with widespread osteoarthritic changes a total knee replacement is usually performed where both the bones forming the knee joint are replaced with prosthetic material and the normal axis and balance of the knee joint is restored to recreate the biomechanics.
Recovery
Post-Surgical Recovery: Post-surgical care is crucial for optimal recovery and may involve:
- Rehabilitation: Begins with gentle exercises to enhance flexibility and strength without overloading the new cartilage. This phase can last from a few weeks to several months.
- Physical Therapy: Focuses on improving joint function, reducing pain, and restoring mobility. Tailored exercises help strengthen the muscles around the knee, providing better support and stability.
Long-Term Care and Lifestyle Adjustments: Maintaining knee health after recovery includes:
- Regular Exercise: Low-impact activities like swimming, cycling, or elliptical training help keep joints flexible and muscles strong.
- Weight Management: Reducing body weight to alleviate stress on the knee.
- Nutritional Support: Diet rich in omega-3 fatty acids, antioxidants, and vitamins can help maintain joint and overall health.
Ongoing Monitoring and Prevention: Regular follow-ups with an orthopedic specialist to monitor recovery and prevent future injuries are essential. This might include periodic imaging to assess the condition of the cartilage repair.
Do you have more questions?
What are the long-term consequences of untreated kneecap maltracking?
Untreated kneecap maltracking can lead to chronic pain, cartilage damage, and increased risk of developing osteoarthritis in the knee joint over time. Seeking early treatment can help prevent these complications.
How common are cartilage injuries in the knee?
Cartilage injuries in the knee are relatively common, especially among athletes and individuals who engage in high-impact activities. They can also occur due to aging and degenerative changes in the joint.
Can cartilage injuries in the knee heal on their own without treatment?
In some cases, minor cartilage injuries may heal on their own with rest and conservative management. However, more significant injuries often require medical intervention to promote proper healing and prevent long-term complications.
Are there any specific risk factors that increase the likelihood of cartilage injuries in the knee?
Yes, several factors can increase the risk of cartilage injuries in the knee, including participating in sports with repetitive knee movements, previous knee injuries, obesity, and genetic predisposition.
How long does it typically take to recover from a cartilage injury in the knee?
The recovery time for a cartilage injury in the knee varies depending on the severity of the injury and the chosen treatment approach. In some cases, individuals may experience improvement within a few weeks, while others may require several months of rehabilitation.
Is surgery always necessary for treating cartilage injuries in the knee?
Surgery is not always necessary for treating cartilage injuries in the knee. Many cases can be effectively managed through conservative treatments such as physical therapy, pain management, and activity modification. However, surgery may be recommended for severe or complex cases.
What are the potential risks and complications associated with surgical interventions for cartilage injuries in the knee?
Surgical interventions for cartilage injuries in the knee carry certain risks and potential complications, including infection, bleeding, nerve damage, and failure of the procedure to provide the desired outcome.
Can cartilage injuries in the knee lead to long-term joint damage or arthritis?
Yes, untreated or improperly managed cartilage injuries in the knee can lead to long-term joint damage and increase the risk of developing osteoarthritis, a degenerative joint disease characterized by cartilage breakdown and inflammation.
Are there any specific exercises or activities that individuals with cartilage injuries in the knee should avoid?
Individuals with cartilage injuries in the knee should avoid high-impact activities and exercises that place excessive stress on the joint, such as running, jumping, and heavy lifting. Instead, they should focus on low-impact exercises and activities that promote joint stability and flexibility.
How can I prevent cartilage injuries in the knee from recurring?
Preventing cartilage injuries in the knee from recurring involves maintaining a healthy weight, participating in regular exercise to strengthen the muscles around the knee joint, using proper techniques during physical activities, and wearing supportive footwear.
Are there any dietary or nutritional recommendations that can help support cartilage health in the knee?
While there is no specific diet that can guarantee cartilage health, consuming a balanced diet rich in nutrients such as vitamin C, vitamin D, calcium, and omega-3 fatty acids can help support overall joint health and reduce inflammation.
Is there a specific age group more prone to cartilage injuries in the knee?
Cartilage injuries in the knee can occur in individuals of all age groups, but they are more common in older adults due to age-related changes in the joint and increased risk of degenerative conditions like osteoarthritis.
Can cartilage injuries in the knee affect other areas of the body besides the knee joint?
While cartilage injuries in the knee primarily affect the knee joint, they can also lead to compensatory changes in gait and movement patterns, potentially causing secondary issues in other areas of the body such as the hips and lower back.
Is there a difference in treatment approaches for acute versus chronic cartilage injuries in the knee?
Yes, the treatment approach for acute (recently occurred) versus chronic (long-standing) cartilage injuries in the knee may vary. Acute injuries may require immediate rest, ice, compression, and elevation (RICE) followed by conservative management, while chronic injuries may necessitate more aggressive interventions such as surgery.
Are there any non-surgical alternatives for managing cartilage injuries in the knee?
Yes, several non-surgical alternatives exist for managing cartilage injuries in the knee, including physical therapy, pain management techniques, regenerative medicine therapies, and lifestyle modifications.
Can cartilage injuries in the knee worsen over time if left untreated?
Yes, cartilage injuries in the knee can worsen over time if left untreated, leading to progressive pain, stiffness, and functional impairment. In severe cases, untreated injuries can result in irreversible joint damage and disability.
How soon after sustaining a knee injury should I seek medical attention?
It is advisable to seek medical attention promptly after sustaining a knee injury, especially if you experience persistent pain, swelling, or difficulty bearing weight on the affected knee. Early intervention can help prevent further damage and improve treatment outcomes.
Is it possible to prevent cartilage injuries in the knee altogether?
While it may not be possible to completely prevent cartilage injuries in the knee, certain preventive measures such as maintaining a healthy weight, staying physically active, using proper techniques during physical activities, and wearing supportive footwear can help reduce the risk.
Are there any specific diagnostic tests that can accurately assess the extent of cartilage damage in the knee?
Yes, diagnostic tests such as MRI (Magnetic Resonance Imaging) and arthroscopy can provide detailed images of the knee joint and accurately assess the extent of cartilage damage. These tests help guide treatment decisions and prognosis.
How does age impact the effectiveness of treatment for cartilage injuries in the knee?
Age can impact the effectiveness of treatment for cartilage injuries in the knee, with younger individuals generally having a better capacity for cartilage repair and regeneration compared to older adults. However, treatment outcomes also depend on factors such as the severity of the injury and overall health status.
Are there any specific precautions I should take during the recovery period after treatment for a cartilage injury in the knee?
During the recovery period after treatment for a cartilage injury in the knee, it is important to follow your healthcare provider’s instructions carefully, including participating in prescribed rehabilitation exercises, avoiding high-impact activities, and attending follow-up appointments for monitoring progress.
Can cartilage injuries in the knee be hereditary or genetic?
While cartilage injuries in the knee are often associated with factors such as trauma, overuse, and aging, there may also be a genetic component that predisposes some individuals to cartilage abnormalities and injuries.
Are there any specific occupational or recreational activities that increase the risk of cartilage injuries in the knee?
Yes, certain occupational or recreational activities that involve repetitive knee movements, heavy lifting, or prolonged standing can increase the risk of cartilage injuries in the knee. Examples include construction work, landscaping, and high-impact sports.
Are there any emerging treatments or technologies for cartilage injuries in the knee that show promise?
Yes, there are several emerging treatments and technologies for cartilage injuries in the knee that show promise, including tissue engineering techniques, 3D printing of cartilage implants, and advanced imaging modalities for early detection and monitoring of cartilage damage.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
