ACL Surgery Complications
Anterior cruciate ligament injuries are common in young athletes as well as middle-aged adults. While anterior cruciate ligament (ACL) injuries may be treated non-surgically, the majority of the patients opt for surgical management of the ACL tears.
The surgical management is usually done in the form of arthroscopic reconstruction. The arthroscopic ACL reconstruction is a very safe surgery but patients may have concerns regarding immediate and long-term complications of the surgery.
What is ACL Surgery? The ACL is a crucial ligament that stabilizes the knee joint. Injuries to this ligament are common, especially among athletes engaged in sports like soccer, basketball, and football. ACL surgery, also known as ACL reconstruction, involves repairing or replacing the torn ACL with a graft to restore knee stability and function.
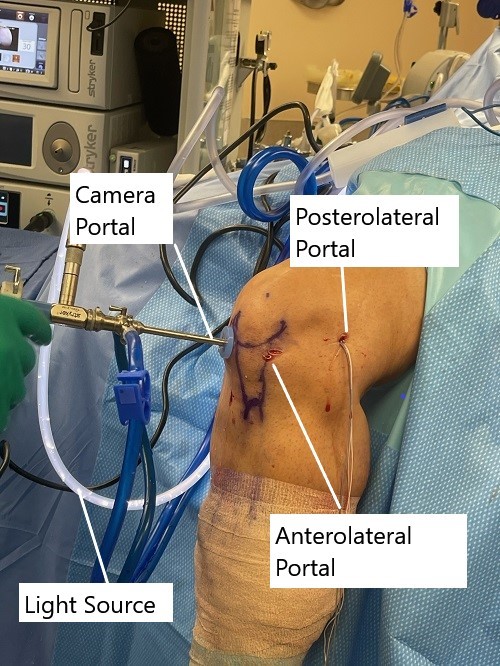
Intraoperative image showing knee arthroscopic ACL reconstruction.
During an ACL reconstruction surgery using an arthroscope, the surgeon harvests a graft from the patient or uses a cadaveric or synthetic graft to replace the torn ligament. The surgery involves the use of key-hole incisions. The surgeon introduces a small camera with a light source through the keyhole incision.
The minute instruments are inserted through another keyhole incision. The surgeon guides the instruments using the arthroscopic camera display on the outside screen. The graft is securely tightened and the knee is placed in a brace. An ACL rehabilitation is started to achieve optimum function and a return to normal activities/sports.
The complication of ACL reconstruction may be summarized as the ones due to pre-operative decisions, intraoperative causes, and postoperative causes.

Implant (screw) used for securing the graft.
Preoperative decisions
- ACL reconstruction is deferred until the swelling has subsided after an acute injury. Performing the surgery too early may lead to knee stiffness after the ACL reconstruction. Generally, ACL reconstruction surgery is deferred until the patient is able to bend (90 degrees) and straighten the injured knee fully.
- Missing of additional injures of the knee structures such as medial collateral ligament, posterior lateral corner injuries and meniscus may lead to instability of the ACL reconstruction and possible graft failure. The patient may complain of continued knee pain and instability after ACL reconstruction. The additional injuries may be recognized with careful physical examination and radiological studies.
- Not performing the ACL surgery when needed and waiting for too long may lead to damage to the articular knee cartilage and meniscus. The patient should be educated regarding the possible risks of non-operative treatment and should be advised to limit activities with continued bracing.
Common Complications:
Infection:
Explanation: Sometimes, germs can enter the surgical site, leading to an infection. This can cause redness, swelling, warmth, and pain in the knee
Management: Prompt treatment with antibiotics and proper wound care are essential to manage infections. In severe cases, surgical drainage may be required.
Why It Happens: Infections can occur due to bacteria entering the body during surgery or post-operative care. Factors such as poor wound care, compromised immune system, or contaminated surgical instruments can increase the risk.
Blood Clots:
Why It Happens: Surgery can disrupt normal blood flow, leading to the formation of blood clots. Factors such as prolonged immobility, obesity, smoking, or a history of blood clots can increase the risk.
Management: Blood thinning medications may be prescribed to prevent clot formation. Moving the legs regularly and wearing compression stockings can also help reduce the risk.
Explanation: Blood clots are clumps of blood that can form in the veins of the leg after surgery. These clots can block blood flow and cause swelling and pain.
Knee Stiffness:
Management: Physical therapy exercises are crucial for regaining range of motion and reducing stiffness. In some cases, additional surgical procedures may be necessary to remove scar tissue.
Why It Happens: Stiffness can occur due to scar tissue formation or inflammation in the knee joint during the healing process.
Explanation: After surgery, some patients may experience stiffness in the knee, making it difficult to bend or straighten fully
Graft Failure:
Management: Revision surgery may be required to replace the failed graft. Rehabilitation protocols may also be adjusted to prevent re-injury.
Why It Happens: Graft failure can occur due to factors such as poor surgical technique, improper graft placement, or inadequate rehabilitation.
Explanation: The graft used to repair the ACL may fail to integrate with the surrounding tissues or may tear again, compromising the stability of the knee.
Nerve Damage:
Why It Happens: Nerve damage can occur due to the surgical incision or manipulation of tissues during surgery
Management: Nerve damage may improve over time with rehabilitation and nerve stimulation techniques. In severe cases, surgery may be necessary to repair the damaged nerves.
Explanation: Surgery can sometimes damage nerves in the knee area, leading to numbness, tingling, or weakness in the leg.
Persistent Pain:
Management: Pain management strategies may include medications, physical therapy, acupuncture, or corticosteroid injections. In some cases, further evaluation may be needed to identify the underlying cause of pain.
Why It Happens: Persistent pain can result from various factors, including nerve damage, graft failure, inflammation, or underlying knee arthritis.
Explanation: Some patients may experience persistent pain in the knee despite surgery, which can affect daily activities and quality of life.
Joint Instability:
Management: Rehabilitation focused on strengthening the muscles around the knee joint is essential for improving stability. In some cases, additional surgical procedures may be necessary to address persistent instability.
Why It Happens: Joint instability can occur due to inadequate graft fixation, ligament laxity, or muscle weakness.
Explanation: Despite surgery, some patients may continue to experience instability or giving way sensations in the knee, making it difficult to engage in physical activities.
Intraoperative complications
- Kneecap (patella) fracture may occur during the surgery when a bone-patellar-tendon-bone (BPTB) graft is taken. The fracture of the kneecap may occur as a result of improper bone cuts during harvesting the graft.
- Improper harvest of the hamstring graft may either lead to a very small graft or may lead to knee bending weakness. Excessive harvest of the hamstring graft may weaken the hamstring muscle and may lead to knee flexion weakness.|
- There may be an inadvertent injury to the saphenous nerve during cutting of the skin and the tissues. The saphenous nerve injury may lead to numbness and tingling over the inner aspect of the knee joint.|
- There is a risk of damage to the major blood vessels and nerves behind the knee that may lead to amputation or paralysis of the foot.|
- ACL graft mismatch may occur as a result of a smaller, longer, wider, or narrower graft as compared to the graft tunnels. The mismatch may cause instability or stiffness of the knee joint.|
- Similarly improper placement of the graft tunnel may lead to instability, loss of knee flexion, loss of knee extension, knee pain, and graft rupture.
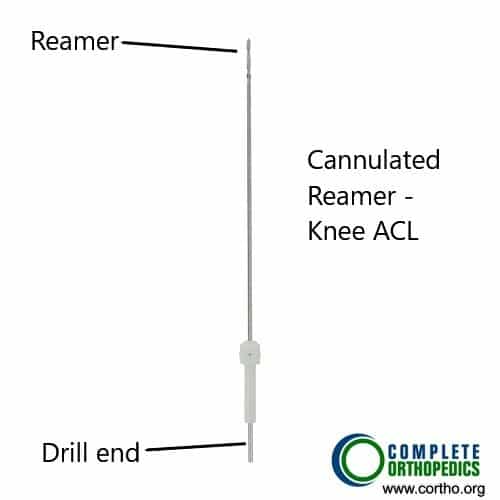
Instruments used to drill the tunnel in ACL reconstruction.
Postoperative complications
- Stiffness is a common post-ACL reconstruction complication that is defined as the incomplete range of motion of the knee following surgery. The complication may be a result of poor technique during surgery or due to poor adherence to post-operative rehabilitation protocol. Aggressive rehabilitation, manipulation under anesthesia, arthroscopic adhesiolysis may be used to relieve knee stiffness.
- Patella fracture after ACL reconstruction may result from graft harvesting. The patella fracture may require surgical management.
- Pain, swelling, redness, the rise of temperature, and stiffness may occur as a result of infection. Radiological and knee aspirate and cultures may be needed for diagnosis. The infection may be managed with thorough lavage, antibiotics, debridement, etc. The management may at times necessitate the removal of the graft.
- Pain in the front of the knee after the surgery is commonly associated with patellar tendon graft but may also occur in cases of allograft and quadriceps tendon graft. The pain may occur due to noncompliance with postoperative rehabilitation protocol.
ACL reconstruction is a safe surgery and the associated complications are rare. Compliance with postoperative rehabilitation protocol ensures a quick return to activities of daily living and sports.
Conclusion
While ACL surgery can effectively restore knee function and stability, it is not without risks. Understanding the potential complications and their management is crucial for patients undergoing ACL reconstruction. By working closely with healthcare professionals and adhering to rehabilitation protocols, patients can optimize their outcomes and minimize the impact of complications on their recovery journey.
Do you have more questions?
How common are infections after ACL surgery?
Infections after ACL surgery are relatively uncommon, occurring in less than 2% of cases. However, proper wound care and infection prevention measures are essential to minimize the risk.
Can infections after ACL surgery be life-threatening?
In most cases, infections after ACL surgery are not life-threatening. However, if left untreated, they can lead to serious complications and may require additional treatment such as surgical drainage or intravenous antibiotics.
What steps can be taken to prevent infections after ACL surgery?
To prevent infections after ACL surgery, it’s crucial to maintain good hygiene, follow your surgeon’s pre-operative and post-operative instructions, and adhere to wound care protocols. Additionally, antibiotics may be prescribed before and after surgery to reduce the risk of infection.
How soon after ACL surgery can blood clots form?
Blood clots can form in the days or weeks following ACL surgery, especially during the initial stages of recovery when mobility is limited. It’s essential to be vigilant for symptoms of blood clots and follow your surgeon’s recommendations for prevention.
Are blood clots after ACL surgery common?
Blood clots after ACL surgery are relatively rare, occurring in less than 1% of cases. However, certain risk factors such as obesity, immobility, and a history of blood clots can increase the likelihood.
What are the symptoms of blood clots after ACL surgery?
Symptoms of blood clots after ACL surgery may include swelling, warmth, redness, and pain in the calf or thigh. If you experience any of these symptoms, you should seek medical attention promptly.
How are blood clots diagnosed after ACL surgery?
Blood clots after ACL surgery are typically diagnosed through a combination of physical examination, ultrasound imaging, and blood tests to measure clotting factors.
Can blood clots after ACL surgery be fatal?
While rare, untreated blood clots after ACL surgery can potentially be fatal if they travel to the lungs and cause a pulmonary embolism. Prompt diagnosis and treatment are essential to prevent serious complications.
What measures can be taken to prevent blood clots after ACL surgery?
To prevent blood clots after ACL surgery, patients are often encouraged to move their legs regularly, wear compression stockings, and take blood-thinning medications as prescribed by their surgeon.
How long do knee stiffness and swelling typically last after ACL surgery?
Knee stiffness and swelling are common after ACL surgery and may persist for several weeks to months, depending on individual factors such as the extent of the injury and the type of surgical technique used.
Can knee stiffness after ACL surgery be permanent?
In most cases, knee stiffness after ACL surgery is temporary and improves with time and rehabilitation. However, in rare instances, persistent stiffness may require further evaluation and treatment.
What can be done to alleviate knee stiffness after ACL surgery?
Physical therapy exercises, stretching, and gentle mobilization techniques can help alleviate knee stiffness after ACL surgery. Your physical therapist will tailor a rehabilitation program to address your specific needs and limitations.
How soon after ACL surgery can I expect to regain full range of motion in my knee?
Regaining full range of motion in the knee after ACL surgery can vary depending on individual factors such as the extent of the injury, surgical technique, and adherence to rehabilitation. In general, patients can expect gradual improvement over several weeks to months.
Are there any warning signs of graft failure after ACL surgery?
Warning signs of graft failure after ACL surgery may include sudden instability in the knee, recurrent giving way episodes, and persistent pain or swelling. If you experience any of these symptoms, you should contact your surgeon for evaluation.
What factors can contribute to graft failure after ACL surgery?
Graft failure after ACL surgery can be influenced by various factors such as poor surgical technique, inadequate graft fixation, premature return to activity, and failure to adhere to rehabilitation protocols.
How common is nerve damage after ACL surgery?
Nerve damage after ACL surgery is relatively rare, occurring in less than 1% of cases. However, certain factors such as the location and extent of the surgical incision can increase the risk.
Can nerve damage after ACL surgery be permanent?
In most cases, nerve damage after ACL surgery is temporary and improves over time with proper rehabilitation and nerve stimulation techniques. However, in severe cases, permanent nerve damage may occur.
How soon after ACL surgery can I expect to regain sensation in my leg?
Sensation in the leg typically returns gradually after ACL surgery as the nerves regenerate. Most patients experience improvement within a few weeks to months, but complete recovery may take longer.
What can be done to manage persistent pain after ACL surgery?
Persistent pain after ACL surgery may be managed through various approaches, including medications, physical therapy, acupuncture, corticosteroid injections, and lifestyle modifications. Your surgeon will work with you to develop a personalized pain management plan.
Are there any long-term complications associated with ACL surgery?
In the long term, most patients experience improved knee stability and function after ACL surgery. However, some may develop complications such as osteoarthritis, persistent pain, or recurrent instability, especially if there are additional injuries or risk factors present.
How soon after ACL surgery can I drive a car?
The timing of driving after ACL surgery depends on several factors, including the type of surgery performed, the leg operated on, and the use of pain medications. In general, patients can resume driving once they feel comfortable and are no longer taking narcotic pain medications. It’s important to consult with your surgeon and adhere to any driving restrictions.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
