Case Study: Lateral Meniscectomy, Chondroplasty, Lateral
Femoral Condyle SubChondroplasty in a 43 year-old female
The shinbone (tibia) is covered in thick, springy bands of cartilage called the medial and lateral meniscectomy. They stabilize the knee and serve as shock absorbers. Size and severity of meniscus tears can vary significantly.
To stabilize and treat chondral lesions, a procedure known as chondroplasty involves removing unstable cartilage flaps and smoothing out degenerating cartilage.
In order to specifically heal chronic BMLs by filling them with a bone replacement substance, sub chondroplasty is a minimally invasive surgery. The bone deficiency is then repaired by gradually resorbing the artificial bone and replacing it with healthy bone.
The patient, a 43 year-old female, came to visit the office with complaints of right knee pain. The patient has received conservative treatment with no benefits.
An MRI revealed a medial meniscus rupture, subcondylar fracture, and microfracture of the lateral femoral condyle. The patient’s lateral femoral condyle was extremely painful. The patient was not weight bearing and so received no benefit.
We discussed treatment alternatives, and the patient decided on surgical intervention. We reviewed risks and benefits such as infection, bleeding, nonhealing, the need for repeat surgery, knee arthritis, the need for rehabilitation, and the necessity for future knee replacement, among other things.
We also talked about systemic concerns such as blood clots, cardiac, neurological, and pulmonary consequences like death. The patient comprehended and signed an informed consent form.
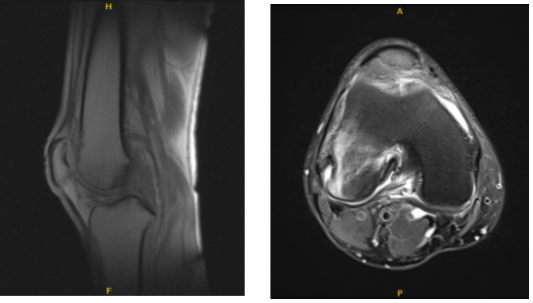
MRI-3T Right knee non-contrast
The patient was brought to the operation room and placed on a well-padded operating table. Anesthesia was administered. A tourniquet was used to stop the bleeding. A preoperative antibiotic was administered. In the usual manner, the right lower extremity was prepped and draped aseptically.
The tourniquet had been inflated. The medial facet of the patella was found to have osteoarthritic lesions. A medial entrance portal was created after inserting the arthroscope into the medial compartment.
An examination of that medial compartment revealed a stable old healed osteochondral lesion on the lateral aspect of the medial femoral compartment. There was no medial meniscus tear.
The ACL was found to be intact when the intercondylar notch was examined. The posterior horn of the lateral meniscus was torn during an examination of the lateral tibiofemoral compartment. Biters and shavers were used to debride the lateral meniscus posterior horn.
The patellofemoral compartment was examined again, and an osteoarthritic lesion of the medial facet of the patella was debrided using a shaver. The arthroscope was inserted via the medial portal, and the findings were reconfirmed before the final images were stored. The emphasis was now on removing the lateral femoral condyle. A fluoroscope was used in the experiment.
A drill hole was created about 2.5 cm proximal and anterior to the inferior and posterior articular surfaces of the femoral condyle under fluoroscopy guidance. It was inserted around 15 mm too.
Another drill hole was created in the lateral femoral condyle with a similar cannula around 0.5 cm proximal and anterior to the previous cannula. Pictures were obtained in the AP and lateral views and were deemed to be good.
Tricalcium phosphate bone cement was prepared and injected around 2.5 milliliters into each cannula. C-arm images revealed that the cement was only in the bone.
The femoral condyle and the intercondylar notch were examined using an arthroscope, and no extravasating bone cement was found. The knee scope was removed, and the knee was thoroughly drained. The cement was allowed to dry.
The cannula was withdrawn when the bone cement had been set for more than 12 minutes. The final image was captured with the fluoroscope and preserved. The wound was cleansed and the knee was completely drained.
The closure was done with #3-0 nylon, and 9 cc of Depo-Medrol (40 mg) was injected into the knee. Dressing materials included 4 x 4, ABD, Webril, and ACE wrap. After the procedure, the patient was supposed to utilize crutches. The patient was extubated and taken to the recovery room in a stable condition.
After one week, the patient is here today for her postoperative visit. X-ray for the right knee has been reviewed. She takes Vit d and calcium; she is working with PT but it is not helping. Her pain has not improved.
We opted to proceed with official physical therapy as well as a home workout regimen for knee rehabilitation after examining treatment choices. During the visit, we reviewed the arthroscopy images and removed the stitches. We will continue to use ice and elevate the knee to reduce swelling and pain.
To limit the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications.
We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress.
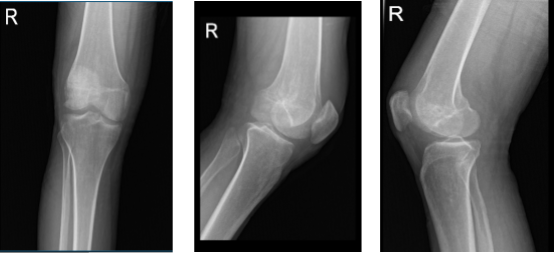
Right knee X-ray AP lateral and oblique 3 views
After one month the patient was seen for her postoperative visit. She takes Vit d and calcium, she is working now with her PT. She is NWB and also uses crutches. We discussed treatment options including PT, MRI, Injection, surgery. We agreed to go with conservative management for now.
Another month has passed since the patient went to the office for her post-operative consultation. She has been improving a lot but has a tender spot on the knee.
The patient decided to proceed with the injection to lessen discomfort and edema after learning about the available treatment choices and the dangers. 40 mg of depo-medrol and 2 injections of 0.5% lidocaine were given after a sterile prep into the right knee trigger point.
There were no issues and the patient tolerated the procedure well. Post-injection discomfort, blood sugar rise, skin pigmentation, fatty atrophy, and infection symptoms were all thoroughly covered. If tolerated, OTC anti-inflammatory medications for discomfort.
The patient seen in the office after three months for her follow up checkup, she is still taking her prescription such as Vit d and calcium and also working with her PT. She is FWB unaided and she got a cortisone injection for a month and it improved her pain.
With continued regular checkup and physical therapy, the patient gets improved gradually, her regular follow up visit every month.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
