KneeCap Maltracking and Management
Knee discomfort is a common experience for many individuals from time to time. However, should this discomfort escalate to a severe level, significantly impacting your daily life, or if you observe symptoms such as swelling, tenderness, or inflammation, seeking advice from a healthcare professional is recommended.
Here at Complete Orthopedics, our team of knee specialists is dedicated to alleviating knee discomfort through a range of treatments, including surgical options when required. Our practice is located in both New York City and Long Island, and we have surgical capabilities in six hospitals, ensuring access to advanced knee surgery and orthopedic care. If you wish to schedule an appointment with one of our orthopedic surgeons, you can easily do so online or by contacting us directly.
Learn about common causes of knee discomfort and the available treatment choices, including situations where surgery emerges as the most suitable course of action.
Overview
Imagine your knee as a well-oiled machine, with bones, muscles, and tendons working together to help you move. At the front of your knee is the kneecap, or patella, which acts like a protective shield for the joint. Kneecap maltracking happens when the patella doesn’t glide smoothly in its groove, causing it to shift or tilt awkwardly during movement. This misalignment can lead to pain, stiffness, and difficulty moving your knee.
If the knee cap (patella) is shifting out of place on bending or straightening it, the person may be dealing with patellofemoral maltracking (PFM).
Anatomy
The knee is the largest joint in your body which is formed of the tibio-femoral and patellofemoral joint. The Patellofemoral joint is formed by the kneecap or Patella sitting over a groove (trochlea) on the lower end of the thigh bone or femur.
It helps in an effective transmission of the forces of the knee movements across the joint. Patellar Maltracking occurs due to an imbalance between the dynamic relationship of the patella and trochlea during the normal range of motion of the knee.
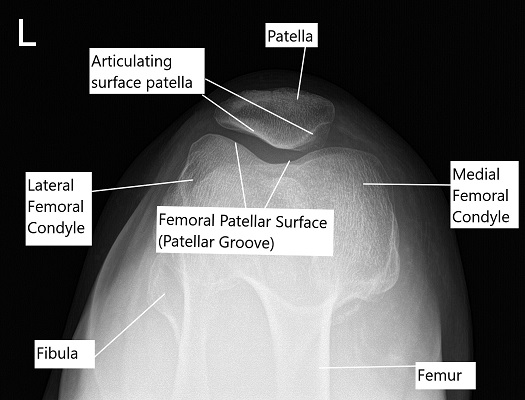
Skyline X-ray view of the patella.
Patellofemoral biomechanics
To understand patellar maltracking first we will have to take a look into understanding how patella helps our leg to bend (flex) and straighten (extend) smoothly. The patellofemoral joint functions as a pulley for the quadriceps muscle to facilitate knee extension and reduce friction.
It is subjected to large amounts of load acting as a pulley. To provide better flexibility and maintain its functions both the bones have ligaments and cartilage to provide support and protection against instability. A small amount of side to side excursion is normally present. Tight tissues(ligaments and tendons) on the inner and outer side of the knee provide stability to the knee cap.
Symptoms
Undue stress on the patellofemoral joint from maltracking will lead to loss and attrition in the articular cartilage of the patellofemoral joint leading to early osteoarthritis with severe limitations of day to day life.
- Anterior Knee Pain: A chronic pain usually in front of the knee.
- Knee Giving Away: Symptoms of knee giving away may be present especially while walking or running. This may be associated with a sensation of grinding or popping every time the knee is moved. When they try to extend their knee it may feel like getting caught or the feeling that the knee won’t support them on standing.
- Episodes of dislocation: At times the patella might dislocate with excruciating pain and swelling. They may be able to relocate the patella by themselves but the episodes become frequent damaging the cartilage.
Causes & Predisposing Factors
Causes of Kneecap Maltracking: Several factors can contribute to kneecap maltracking, including:
Age: As we get older, the cartilage in our knees may wear down, affecting how the patella moves.
Muscle Weakness: Weakness or imbalance in the muscles around the knee can pull the patella out of alignment.
Anatomical Factors: Some people are born with differences in the shape or alignment of their knee joints, making them more prone to maltracking.
Traumatic Injuries : Athletes and people who are physically active may suffer from injuries surrounding the knee cap which is why patellar maltracking disorder often affects young active adults. Often chronic overuse with underlying loss of structural support will lead to patellofemoral maltracking.
Hereditary dysplastic knee cap : People may have a inherited malformed/dysplastic knee cap or the Trochlea. The dysplastic bone does not move into the set tract leading to instability
Patella Alta : A high riding patella (Patella Alta) often leads to instability and maltracking. These patients often have a generalised inherited joint laxity.
Others : bow legs (genu valgum), congenital intoeing (increased femoral anteversion, tibial torsion), tight or lax stabilizing structures on either side of the patella cause patellofemoral maltracking.
Diagnosis
Early diagnosis is essential to prevent or stop the progression of cartilage loss and osteoarthritis.
- History : A detailed history about the clinical symptoms and restrictions of activity is taken.
- Physical Examination : For the physician to understand the dynamic movement of the patella commonly referred to as Patellar Tracking a thorough physical examination of the knee becomes necessary. The physician will conduct some clinical tests and take measurements.
- Q Angle : Q angle is an imaginary angle between the thigh and the patella which is used to measure the degree of patellar engagement in the trochlea. Increased Q angle is usually associated with PFM.
- Imaging : Assessment includes radiograph (x-ray) which is helpful in acute presentation. MRI and CT imaging may be needed and are superior modalities in looking for predisposing factors. MRI allows detailed evaluation of the morphology and structure of the joint especially helpful in guiding operative management.
Treatment
The goal is to recreate the stable dynamic relationship between the patella and the trochlea with a knee which is pain free. Many different approaches have been advocated for treatment. Management can be nonoperative or operative which depends on the severity of the disease.
Non-Surgical Management
Nonoperative treatment generally consists of the use of anti-inflammatory medications, a short period of immobilization, followed by a focused physiotherapy regime with emphasis on range of motion, closed chain exercises, and vastus medialis obliquus (VMO) strengthening.
Recurrent patellar instability still occurs in between 15 and 45% of patients treated nonoperatively. Also the patients return to active sports can be as low, leaving many patients searching for further management options.
Operative Management
Operative management can be categorized as soft tissue procedures i.e not involving the bony structures and bony procedures.
Soft tissue Surgeries
Soft tissue procedures are used to repair or tighten loose and stretched soft tissues or release of the tight ligaments that contribute to patellar instability. They are best indicated in isolation in the setting of recurrent instability with minimal underlying bony malalignment.
Lateral Release :
A commonly used procedure is lateral release which is a knee arthroscopic surgery. Surgery is performed through small incisions and the tight ligament on the outer knee cap is released so as to allow the knee cap to settle towards the inside of the trochlea.
Medial PatelloFemoral Ligament (MPFL) Repair
Reconstruction of the Medial Patellofemoral Ligament (a ligament stabilising the inner side of patella preventing outward dislocation) is a procedure usually done for recurrent lateral patellar instability. The ligament provides vital inner side support to the patella. The ligament is tightened to provide stability to the knee cap.
Bony Procedures
When the underlying cause is bony malalignment, procedures such as:
- Osteotomy : Tibial tubercle (part of tibia providing attachment to patellar tendon) transfer osteotomy can be performed. It involves cutting of the bone and changing the insertion of the patellar tendon, the procedure ultimately affect the position of patella engaging in the trochlea during range of motion. It also prevents the damaged articular cartilage from coming in contact therefore reducing pain and increasing stability.
- Trochleoplasty : Lastly a procedure known as trochleoplasty may be indicated in the patient with significant trochlear dysplasia/malformation causing PFM. This procedure involves altering the shape of the trochlea so that the patella engages in the trochlea effectively during the range of motion.
If you have any above said symptoms or may think you’re suffering from patellar maltracking disorder, consider visiting an orthopaedic surgeon with expertise in knee arthroscopy.
Recovery
Recovering from kneecap maltracking involves a multifaceted approach aimed at relieving pain, restoring normal knee function, and preventing future issues. Let’s explore the recovery process in layman’s terms:
Rest and Protection: After a diagnosis of kneecap maltracking, your healthcare provider may recommend resting the affected knee and avoiding activities that aggravate pain. This might mean taking a break from high-impact exercises like running or jumping to give your knee time to heal. Using supportive braces or taping techniques can also help protect the knee joint during this initial phase of recovery.
Physical Therapy: Physical therapy plays a crucial role in rehabilitating a knee affected by maltracking. A skilled physical therapist will design a personalized exercise program to strengthen the muscles around the knee, particularly the quadriceps and hamstrings. These exercises help correct muscle imbalances and improve the alignment of the patella within its groove. Additionally, the therapist may incorporate stretching exercises to improve flexibility and range of motion in the knee joint.
Modalities for Pain Relief: To manage pain and inflammation associated with kneecap maltracking, your healthcare provider may recommend modalities such as ice therapy, heat therapy, or transcutaneous electrical nerve stimulation (TENS). These modalities can help alleviate discomfort and promote healing in the affected area.
Activity Modification: During the recovery period, it’s essential to modify activities that put excessive stress on the knee joint. Your healthcare provider may advise you to avoid activities like squatting, kneeling, or prolonged sitting with the knees bent. Instead, focus on low-impact exercises like swimming or cycling that provide cardiovascular benefits without straining the knees.
Gradual Return to Activity: As your knee begins to heal and strengthen, your healthcare provider will guide you through a gradual return to your normal activities. This may involve starting with gentle exercises and gradually increasing intensity and duration as tolerated. It’s essential to listen to your body and avoid pushing through pain during this phase of recovery.
Long-Term Management: Once you’ve completed the initial phase of recovery, it’s crucial to maintain a proactive approach to knee health. This includes continuing with prescribed exercises to keep the muscles around the knee strong and flexible. It’s also essential to maintain a healthy weight and avoid activities that put excessive strain on the knee joint to prevent recurrence of maltracking.
Follow-up Care: Regular follow-up appointments with your healthcare provider are essential to monitor your progress and address any lingering concerns. Your provider may recommend periodic check-ups to assess your knee function and make adjustments to your treatment plan as needed.
Conclusion
Kneecap maltracking can be a frustrating and painful condition, but with the right treatment, you can find relief and get back to doing the things you love. Whether you’re exploring non-surgical options like physical therapy and medication or considering surgery, it’s essential to work with a qualified medical team who can guide you through the process. By understanding your condition and taking an active role in your treatment, you can take the first steps toward a healthier, happier life with your knees.
Do you have more questions?
How do I know if I have kneecap maltracking?
If you experience symptoms such as pain around the kneecap, popping sensations, swelling, instability, or difficulty moving your knee, you may have kneecap maltracking. It’s essential to consult with a doctor for a proper diagnosis.
Can kneecap maltracking get better on its own?
In some cases, mild kneecap maltracking may improve with rest, ice, and over-the-counter pain medications. However, if symptoms persist or worsen, it’s important to seek medical attention for proper evaluation and treatment.
Is kneecap maltracking a common condition?
Yes, kneecap maltracking is relatively common, especially among athletes and individuals who engage in activities that put stress on the knees. It can also occur due to aging, injury, or structural factors.
Are there any exercises I can do to help with kneecap maltracking?
Yes, physical therapy exercises focused on strengthening the muscles around the knee, improving flexibility, and correcting muscle imbalances can help alleviate symptoms of kneecap maltracking and improve patellar alignment.
How long does it take to recover from surgery for kneecap maltracking?
Recovery time after surgery for kneecap maltracking can vary depending on the type of procedure performed and individual factors such as age and overall health. Generally, it may take several weeks to months to fully recover and resume normal activities.
Can kneecap maltracking be prevented?
While some factors contributing to kneecap maltracking, such as aging and anatomical differences, cannot be prevented, maintaining a healthy weight, staying physically active, and avoiding activities that put excessive strain on the knees can help reduce the risk.
Will wearing a knee brace help with kneecap maltracking?
Knee braces or straps can provide support and stability to the knee joint, helping to keep the patella aligned during movement. They may be recommended as part of a comprehensive treatment plan for kneecap maltracking.
Are there any specific risk factors for developing kneecap maltracking?
Some factors that may increase the risk of developing kneecap maltracking include previous knee injuries, participation in sports that involve repetitive knee movements (such as running or jumping), and certain anatomical variations in the knee joint.
Can I continue to exercise with kneecap maltracking?
Depending on the severity of your symptoms, you may be able to continue exercising with modifications. It’s important to consult with a healthcare professional or physical therapist to develop a safe and effective exercise plan tailored to your needs.
How do I find a qualified orthopedic knee surgeon to treat kneecap maltracking?
You can start by asking your primary care doctor for recommendations or researching online for orthopedic surgeons specializing in knee conditions. It’s essential to choose a surgeon with experience and expertise in treating kneecap maltracking.
Will I need physical therapy after surgery for kneecap maltracking?
Physical therapy is often an essential part of the recovery process after surgery for kneecap maltracking. A physical therapist can help you regain strength, flexibility, and range of motion in your knee and ensure a smooth recovery.
What are the potential risks and complications of surgery for kneecap maltracking?
Like any surgical procedure, surgery for kneecap maltracking carries risks, including infection, blood clots, and nerve damage. Your surgeon will discuss these risks with you and take steps to minimize them during the procedure.
Can kneecap maltracking affect other joints in the body?
While kneecap maltracking primarily affects the knee joint, it can also lead to compensatory changes in other joints, such as the hips or ankles, as the body tries to adapt to altered movement patterns. Addressing kneecap maltracking early can help prevent these secondary issues.
Will losing weight help improve kneecap maltracking symptoms?
Maintaining a healthy weight can help reduce stress on the knee joint and may alleviate symptoms of kneecap maltracking, especially if excess weight is contributing to the problem. However, weight loss alone may not resolve the issue entirely, and additional treatments may be needed.
Is there a specific age group most commonly affected by kneecap maltracking?
Kneecap maltracking can affect individuals of all ages, but it is more common among adolescents and young adults, particularly those involved in sports or activities that place strain on the knees. However, it can also occur in older adults due to age-related changes in the knee joint.
Can kneecap maltracking be caused by overuse injuries?
Yes, repetitive movements or overuse of the knee joint, such as in certain sports or occupations, can contribute to the development of kneecap maltracking. It’s important to incorporate rest and proper conditioning techniques to prevent overuse injuries.
How soon after surgery can I expect to see improvements in my kneecap maltracking symptoms?
The timeline for improvement after surgery for kneecap maltracking can vary depending on the individual and the specific procedure performed. While some patients may experience relief from symptoms relatively quickly, others may require more time for full recovery and resolution of symptoms.
Can physical therapy alone correct kneecap maltracking without surgery?
In many cases, physical therapy and conservative treatments can effectively manage kneecap maltracking and alleviate symptoms without the need for surgery. However, the success of non-surgical interventions depends on factors such as the severity of the condition and the individual’s response to treatment.
Are there any alternative or complementary treatments for kneecap maltracking?
While physical therapy and conservative treatments are the mainstays of management for kneecap maltracking, some individuals may find relief from complementary therapies such as acupuncture, massage therapy, or chiropractic care. It’s essential to discuss these options with your healthcare provider to ensure they are safe and appropriate for your condition.
Can I return to sports or high-impact activities after surgery for kneecap maltracking?
The ability to return to sports or high-impact activities after surgery for kneecap maltracking will depend on factors such as the type of surgery performed, the individual’s recovery progress, and their overall physical condition. Your surgeon and physical therapist will provide guidance on when it is safe to resume such activities.
Are there any specific exercises or activities I should avoid if I have kneecap maltracking?
While it’s essential to stay active to maintain overall joint health, individuals with kneecap maltracking may need to avoid certain activities that exacerbate symptoms, such as high-impact sports or exercises that place excessive stress on the knees. Your healthcare provider can help you identify safe and effective exercises for your condition.
Can kneecap maltracking be hereditary?
While there is no direct evidence linking kneecap maltracking to specific genetic factors, there may be a genetic predisposition for certain anatomical variations in the knee joint that contribute to the condition. Further research is needed to better understand the genetic factors underlying kneecap maltracking.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
