Case Study: Shoulder Arthroscopic Rotator Cuff Repair
with Rotation Patch and Subacromial Decompression
in a 56 year-old woman
Subacromial decompression is an arthroscopic operation used to loosen the coracoacromial arch’s tight ligament and shave away some of the acromion’s undersurface. This lifts the roof of the shoulder, giving the rotator cuff tendons greater room to move underneath. The subacromial space is then opened by subacromial decompression.
The patient, a 56-year-old woman, came into the clinic complaining of right shoulder ache following a car accident. She attempted physical therapy and painkillers but received no relief. An MRI revealed a partial-thickness right shoulder rotator cuff injury.
We spoke about our alternatives for treatment and decided on surgical treatment. We talked about potential risks and issues, such as bleeding, infections, failure, the requirement for additional surgery, and the requirement for rehabilitation, among others. We talked about systemic issues, such as blood clots and cardiac, pulmonary, and neurological issues. The client was aware and gave informed consent.
The anesthesia team administered a supraclavicular block in the pre-op area. A well-padded operating table was used when the patient was brought into the operating room. After being given sedation, she was positioned with her right shoulder up and her left shoulder lateral.
Well-padded bony prominences on all sides. The bean bag kept her firmly in place. A roll of the axilla was inserted. The right shoulder was prepared as normal and wrapped aseptically. A timeout was ordered. An antibiotic was administered before the surgery.
Because it was difficult to reach the glenohumeral joint through the soft spot, an arthroscope was introduced into the subacromial region. The MRI revealed no disease in the glenohumeral joint. The subacromial area was examined and found to have subacromial bursitis, which was debrided with a shaver.
The supraspinatus has partial thickness ripping around its insertion into the larger tuberosity. Anterior acromial spurring with impingement was seen. A coblation wand was used to loosen the coracoacromial ligament as well as to clean and prepare the acromion for acromioplasty.
The acromial spur was removed with a bur, and the acromioplasty was performed. It was decided to reconstruct the supraspinatus tendon with a Regeneten medical rotation implant. It was introduced via the lateral portal.
To place the tacks, an auxiliary superior gateway was created. It was attached to the rotator cuff tendon with PLLA tacks placed in the tendon region. Two bony tacks were used to secure it over the bone. The final photographs were shot and preserved.
The shoulder had been watered and drained completely. Layers of 2-0 Vicryl and 3-0 nylon were used to close the gap. Adaptic, 4 x 4’s, ABD, and tape were used for dressing. In stable condition, the patient was placed in a shoulder sling and transported to recovery.
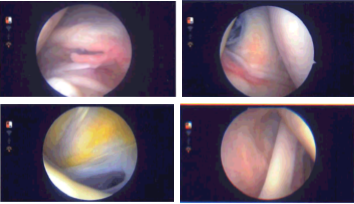
Intraoperative Arthroscopy Images
The patient was seen by the doctor after one week for her postoperative visit, no x-rays needed. She is in the office without a sling and she is doing well; her pain has improved. We chose to proceed with a home workout regimen for shoulder rehabilitation after discussing therapy choices.
During the visit, we removed the stitches. We will continue to use ice and elevate the shoulder to reduce swelling and pain. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications. We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress.
After a month, the patient went to the office for her postoperative visit, no x-rays needed. She is in the office without a sling and is doing well. Instead, she is complaining of worsening pain on the outer shoulder and arm up to the outer wrist with tingling and numbness.
We decided to use cautious management for the time being. PT will start. To lessen discomfort and swelling, we will still utilize ice and elevation, and we will keep taking over-the-counter anti-inflammatory medications. Her follow-up 4 weeks later. Two months have passed, the patient seen in the office for her post operative visits, no x-rays needed.
She went to the office without a sling and doing well, her pain is controlled and more improving. She is improving gradually with PT. The patient’s progress and development have been undeniable with continued physical treatment and regular attendance at his follow-up checkups.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
