Case Study: Management of a 55-year-old Male
with Meniscus Tear and Subchondral Fracture
A 55-year-old male was being followed up in the outpatient clinic for right knee pain for the past year. He works as a chef and had reported a twisting injury to the knee about a year ago. The patient complains of dull deep knee pain and a sharp pain located on the inner side of the knee and just below the knee. The pain is constant and he had recently stopped working secondary to pain as his job entailed him standing most of the time.
The patient described the pain as moderate to severe in intensity. The patient denies any radiation or any associated numbness and tingling with the pain. The patient states that the pain is worse since it started. He had previously tried physical therapy and medications in the form of NSAIDs.
The patients had two cortisone knee injections in the past year. The injections helped alleviate the pain but the relief did not last long. He is a lifetime non-smoker and denies the use of any illicit drugs. The patient’s medical history is significant for diabetes mellitus and hyperlipidemia. His current medications include simvastatin and metformin. He denies any known drug allergy.
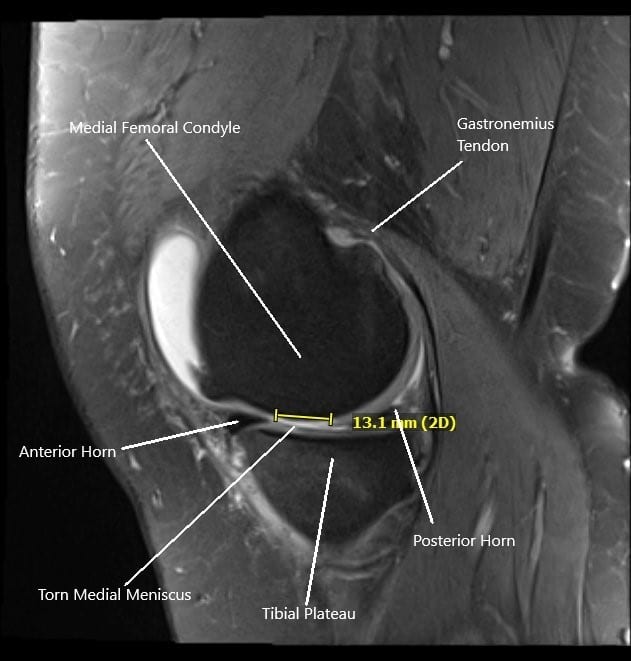
MRI of the right knee in sagittal section showing tear of the medial meniscus.
On examination of the right knee, there is tenderness to palpation on the medial joint line and the medial tibial tubercle. Tenderness is also elicited on deep palpation of the Medial Tibial condyle. The range of motion is limited by pain with flexion of 120 degrees and extension of 0 degrees. McMurray’s and Apley’s compression tests were positive.
MRI of the right knee suggested a complex tear of the posterior horn of the medial meniscus, tibial subchondral stress fracture, and severe patellofemoral arthrosis. Due to the failure of the conservative management, the patient was advised surgical management. Risks, benefits, and potential complications were all discussed at length with the patient. The patients agreed to go ahead with the procedure.
PREOPERATIVE DIAGNOSES:
- Medial meniscus tear of the right knee.
- Medial tibial subchondral fracture, right knee.
POSTOPERATIVE DIAGNOSIS:
- Medial meniscus tear of the posterior horn, right knee.
- Grade 3 to grade 4 chondral lesions of medial femoral condyle, trochlea, patella, grade 1 to grade 2 lesions of the lateral femoral condyle.
- Medial tibial plateau subchondral fracture.
OPERATIONS:
- Right knee arthroscopic medial meniscectomy.
- Right knee arthroscopic chondroplasty of the medial femoral condyle, lateral femoral condyle, PF joint.
- Medial tibial plateau fracture fixation using calcium phosphate cement by subchondroplasty technique.
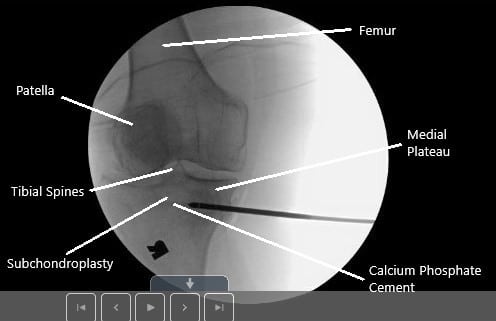
Intraoperative fluoroscopic image of subchondroplasty.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. The right lower extremity was prepped and draped aseptically in the usual fashion. A time-out was called. The preoperative antibiotic was given. Tourniquet was inflated.
A lateral entry portal was made and an arthroscope entered. Examination of the knee showed a large osteochondral grade 3 to grade 4 lesions of the medial femoral condyle. A medial entry portal was made. A complex tear of the posterior horn of the medial meniscal was found.
Debridement of the medial meniscus tear was done using a biter as well as a shaver. Once the medial meniscus tear was adequately balanced, the scope was entered into the intercondylar notch. The ACL was found to be intact. There was degeneration of the ACL.
The lateral compartment was examined and found to have medial fraying and tearing of the lateral meniscus. Shaver was used to cleaning up the meniscus. There was small grade 1 to grade 2 osteochondral lesions of the lateral femoral condyle, which were cleaned using a shaver.
The scope was entered in the patellofemoral joint where grade 3 to grade 4 changes were found in the inferior medial and lateral facet of the patella as well as trochlea. Debridement was done. The knee was again examined from the medial entry portal and findings confirmed.
Now, the attention was moved to the fixation of the stress fracture of the medial tibial plateau. The cannula was entered from the subchondroplasty set medially under C-arm control about a centimeter below the joint surface. It was inserted in an anterolateral direction.
The cannula was checked in AP and lateral view and found to be in adequate position. The subchondroplasty calcium phosphate cement was inserted using 1 cc syringes. Five syringes were used.
The cement could be seen filling up the medial tibial plateau region superiorly, superior to the cannula. Ten minutes were given for the cement to set. The cannula was removed. The final picture was taken and saved.
The wounds were closed using #3-0 nylon. The wounds were dressed using Xeroform, 4 x 4, Webril, and Ace wrap. The patient was moved to recovery after extubation in stable condition. The patient is to be toe-touch weight bearing using crutches.
The patient had an excellent recovery post-op and continues to follow up in the clinic.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
