The patient was seen by me in the office with complaints of shoulder pain following an accident. His X-ray showed No abnormal soft tissue calcification is present.
Acromioclavicular joint reveals no significant abnormalities. The patient was treated conservatively, but failed. An MRI was done, which showed a rotator cuff tear of the left shoulder.
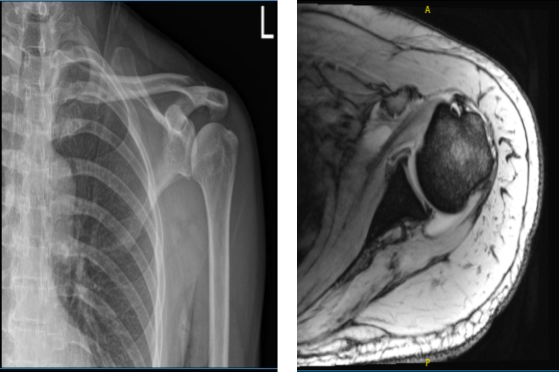
MRI of the left shoulder
We discussed treatment options and the patient opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, failure of repair, need for rehabilitation, need for repeat surgery, among others. We also discussed systemic complications.
The patient understood and signed an informed consent.
The patient was taken to the operating room where general anesthesia was induced. The patient was put in the right lateral position with the left shoulder up. All bony prominences were well padded. Axillary roll was inserted in the axilla. The patient was positioned in a sloppy lateral with the use of a bean bag.
He was well taped to the bag. Preoperative antibiotic was given. The left shoulder was prepped and draped aseptically in the usual fashion with a 10-pound traction in 45 degrees of abduction and flexion. The posterior entry portal was made. Time-out was called.
The posterior entry portal was made through the soft spot. The arthroscope was entered. There was deep labeled degeneration and tearing around the superior labrum as well as the anterior labrum and the posterior labrum.
The debridement was done with the shaver through the anterior entry portal, which was made using a spinal needle. Biceps were found to be intact. There was no biceps tendonitis. There was a large rotator cuff, it could be seen through the glenohumeral joint.
It was decided to approach the subacromial space and repair it. After the debridement of the glenohumeral joint, the arthroscope was entered into the subacromial space. Shaver was entered through the anterior portal to the subacromial bursitis, which was cleaned using a shaver.
Lateral entry portal was made. Arthroscope was entered from there and subacromial decompression was completed. The rotator cuff was delineated and debrided. It started right at the biceps tendon and continued into the infraspinatus.
It was decided to do the repair of the rotator cuff using four-tail anchors of Arthrex. Two anchors were inserted through along the lateral margin of the acromion anterior and posterior aspects after preparing the humeral head. The sutures were passed sequentially x4 through the rotator cuff.
An accessory portal was made to achieve the passage of the sutures. The sutures were not yet to reach onto itself. Finding it to be an appropriate reduction of the rotator cuff and adequate repair, the suture was clipped.
Acromioplasty was then performed using a burr. Distal clavicular excision was performed using a burr and about 1 cm of missed pedicle was excised. Final pictures were taken and saved.
The shoulder was thoroughly irrigated. The shoulder was drained and closed with nylon # 4-0. Locals were instilled. Dressing was done using Adaptic, 4x8s, ABD, tape. The patient was extubated and moved to a recovery area in stable condition.
After two weeks the patient is seen in the office for follow up checkup, the patient is doing well after the surgery, he has no other signs and symptoms and we decided to discuss the treatment options.
We will proceed with the formal physical therapy as well as a home exercise program for rehabilitation of the shoulder. We removed the stitches during today’s visit. We will continue with ice and elevation of the shoulder to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking this medication. the three weeks’ time to evaluate their progress.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

