Partial vs Total Knee Replacement
If knee pain becomes severe enough to disrupt daily activities or is accompanied by swelling, tenderness, or redness, it’s important to consult a doctor.
At Complete Orthopedics, our expert knee doctors specialize in managing knee pain through both non-surgical and surgical options. We evaluate symptoms, identify problems, and devise suitable treatment plans, which may include surgery.
With facilities in New York City and Long Island and connections to six hospitals, we offer cutting-edge knee surgery and complete orthopedic care. You can book an appointment with our orthopedic surgeons either online or via telephone.
Discover the typical causes and treatments for knee pain and learn when surgery is the most effective solution.
Overview
Knee replacement surgeries are safe and effectively manage the pain and disability caused by osteoarthritis. During knee replacement surgery, the ends of the diseased joint are replaced with prosthetic metal and plastic parts.
While in total knee replacement all the compartments of the knee joint are usually replaced, a partial knee replacement only involves the replacement of a single knee compartment.
The knee joint is divided into three compartments or spaces. The joint is formed by the lower end of the thigh bone, the upper part of the shinbone, and the undersurface of the kneecap.
The inner side of the knee is called the medial compartment, and similarly, the outer side of the knee forms the lateral compartment. In front of the knee, the joint formed by the kneecap and the thigh bone forms the patellofemoral compartment.
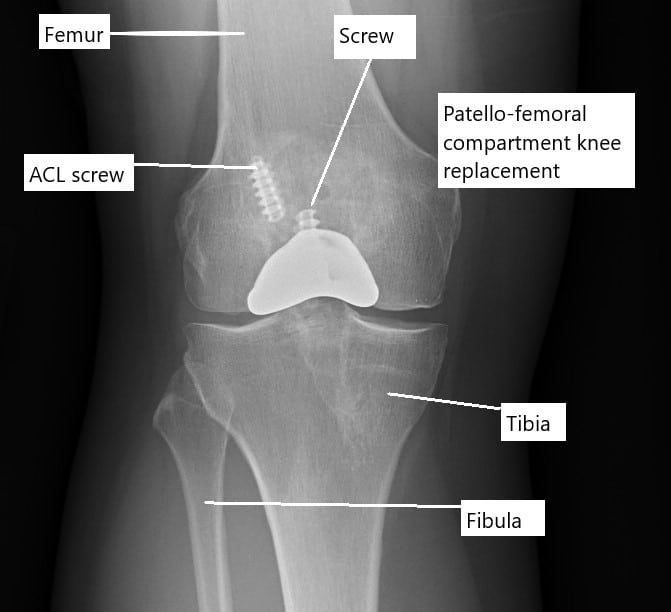
X-ray showing a partial knee replacement.
The bones forming the knee joint are covered with a glistening white tough tissue known as articular cartilage. The articular cartilage helps in the smooth gliding of the joint in motion. Various ligaments, meniscus, and muscles provide additional stability to the knee joint.
Majority of the patients who may need joint replacement surgery suffer from osteoarthritis. Osteoarthritis is a wear and tear disease of the joint that gradually destroys the articular cartilage, the bone ends, and the ligaments secondary to instability. Arthritis may affect all the compartments at the same time or may start in one of the compartments first.
Patients with knee arthritis may complain of pain, stiffness, or deformity. A knee replacement surgery is only offered to the patients when all other nonsurgical treatments have been tried. Nonsurgical treatments include physical therapy, cortisone injections, and pain medications, etc.
Partial knee replacement
In a partial knee replacement, only one of the compartments of the knee is replaced. During a partial knee replacement surgery, the surgeon accesses the joint through a usually smaller incision. The diseased ends of the bones forming the compartment are then cut to be removed. All the ligaments and other soft tissue structures are left intact.
A metal prosthetic component is placed on the cut bony ends and fixed with bone cement. A high-grade plastic part is placed in between the metal parts for the smooth gliding of the metal surfaces. The incision is closed in layers and the patient is able to walk the same day of the surgery.
Not all patients are candidates for partial knee replacement. The partial replacement surgery is only recommended in the following patients:
- Patients with evidence indicating the involvement of only one compartment of the knee joint.
- The knee joint is stable without any damage to the ligaments such as the anterior cruciate ligament, posterior cruciate ligament, or medial and lateral collateral ligaments.
- Patients with no history of meniscus surgery in the other compartment.
- Generally, patients aged 60 or more with less demanding lifestyles who are not obese.
- Patients with no evidence or history of inflammatory arthritis such as rheumatoid arthritis, reactive arthritis, etc.
- Patients with no significant deformity of the knees such as bow legs, knock knees, flexion deformities, or inability to bend the knee more than 90 degrees.
Partial vs Total Knee
Since the partial knee replacement involves the replacement of only one of the knee compartments, the surgery time is significantly less than the total knee replacement. The risk of complications associated with a knee replacement surgery such as blood loss, nerve damage, deep vein thrombosis, infection, etc is also less in the case of a partial knee replacement.
Since less tissue and bone are cut and the ligaments are left intact, a partial knee replacement has a more natural feeling to the knee joint. Comparatively, patients who undergo total knee replacement often complain of feeling unnatural mechanical knees. The unnatural feeling is a result of the removal of the ligaments of the knee that carry nerve sensations to the brain.
Patients undergoing partial knee replacement are able to get back to their daily activities sooner than total knee replacement. As significantly less cutting is involved in a partial knee replacement, the patients experience less postoperative pain and are able to participate in rehabilitation sooner.
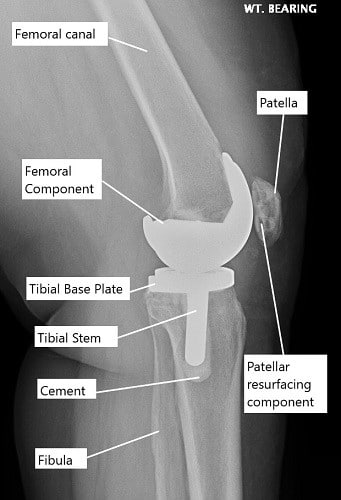
X-ray showing a total knee replacement.
Partial knee replacement however is not frequently done even in patients with unicompartmental knee arthritis as:
- In the majority of cases, a partial knee replacement may need revision surgery in the form of a complete knee replacement. Arthritis eventually may involve the other compartments of the knee causing pain and deformity.
- The revision surgery to total knee replacement from a partial joint replacement is often more complicated than a primary total knee replacement surgery.
- A number of patients with knee arthritis have deformities such as knock knees, bow-legs, or inability to completely straighten or bend the knee. The deformity can be easily corrected in a total knee replacement leading to better knee kinematics.
- Any subsequent ligament or meniscus damage in a patient with a partial knee replacement surgery may require a revision into a total knee replacement.
- Inflammatory arthritis usually involves the entire joint instead of a single compartment. Patients with inflammatory arthritis are more effectively managed with a total knee replacement surgery.
Total knee replacement surgery has revolutionized the management of knee arthritis. Patients today prefer an early joint replacement surgery after failure of non-surgical methods due to the drastic improvement in quality of life with regained mobility.
The majority of the patients who may be candidates for a partial knee replacement generally opt for a total knee replacement due to lower revision rates.
Decision Factors for PKR vs. TKR
The choice between PKR and TKR often depends on several factors:
- Extent of arthritis: TKR is necessary if multiple compartments of the knee are affected.
- Patient’s age and activity level: Younger, more active patients may benefit from the natural knee feel of a PKR, whereas older patients with less demanding daily activities might be better candidates for TKR.
- Overall health: Patients with other health issues might opt for PKR to reduce the time under anesthesia and minimize hospital stay.
Rehabilitation and Recovery
Rehabilitation is crucial for both procedures. It typically involves physical therapy to restore knee function and strengthen the muscles around the knee. The goal is to return to normal activities as safely and quickly as possible.
Long-Term Considerations
Long-term outcomes of knee replacement surgeries are generally positive, with many patients experiencing significant pain relief and improved mobility. Regular follow-ups and monitoring are essential to ensure the longevity of the implant and address any complications should they arise.
Conclusion
In summary, the decision between PKR and TKR should be made based on a thorough assessment by an orthopedic surgeon, considering the specific needs and conditions of the patient. Each procedure has its advantages and disadvantages, and the right choice varies from patient to patient based on individual factors and the extent of knee damage. Both surgeries have high success rates in alleviating pain and restoring function, greatly enhancing the quality of life for patients with debilitating knee conditions.
Do you have more questions?
Are there any age restrictions for either PKR or TKR?
There are no strict age restrictions for either procedure. The decision is more dependent on the patient’s overall health, activity level, and the extent of joint damage rather than age alone.
How long do the implants from a PKR and TKR last?
Knee replacement implants can last 15-20 years or more, but longevity can vary based on factors like the patient’s activity level, weight, and the accuracy of the implant placement during surgery.
What is the risk of infection with knee replacement surgery?
The risk of infection is low, typically around 1-2% for knee replacements. Hospitals take numerous precautions to prevent infections, including antibiotics before and after surgery.
Can I undergo a PKR if I have had previous knee surgeries?
Yes, you can still be a candidate for PKR after previous knee surgeries, depending on the condition of your knee and the type of surgeries performed. Each case needs to be evaluated individually.
What are the signs that I might need a TKR instead of a PKR?
You might need a TKR if you have severe arthritis affecting more than one compartment of the knee, significant stiffness, or you have had previous surgeries that have not successfully alleviated pain.
What is the typical recovery time for PKR versus TKR?
Recovery can vary, but generally, patients recover faster from PKR, often resuming normal activities within 4-6 weeks. TKR recovery might take 8-12 weeks or longer.
What kind of anesthesia is used during these surgeries?
Both surgeries can be performed under general anesthesia, where you are completely asleep, or spinal anesthesia, where you are awake but numb below the waist.
Are there any non-surgical alternatives to knee replacement?
Yes, non-surgical options include weight management, physical therapy, anti-inflammatory medications, corticosteroid injections, and viscosupplementation injections.
How do I know if my arthritis is suitable for PKR?
An orthopedic surgeon can determine if your arthritis is limited to one compartment with a physical exam and imaging tests like X-rays or MRI.
What happens during TKR surgery?
In TKR surgery, all three compartments of the knee are replaced with prosthetic components to create new joint surfaces.
What is the success rate of PKR and TKR?
Both surgeries have high success rates, with many patients experiencing significant pain relief and improved mobility. Success rates can exceed 90% depending on the circumstances and the surgeon’s expertise.
Can I play sports after knee replacement?
While high-impact sports are generally not recommended after knee replacement, many patients can return to low-impact activities like swimming, cycling, and golf.
What is the risk of dislocation with PKR and TKR?
The risk of dislocation is more relevant to hip replacement. For knee replacements, the concern is not dislocation but rather implant loosening or wear over time.
How do I prepare for knee replacement surgery?
Preparation typically involves several preoperative tests, discussions about anesthesia, and possibly banking your own blood for transfusion if needed. It also involves planning for postoperative care and rehabilitation.
What are the major risks associated with knee replacement surgery?
Major risks include infection, blood clots, implant failure, and complications from anesthesia, although these are relatively rare.
How long will I stay in the hospital after surgery?
The stay can vary; PKR patients may go home the same day or after one night, while TKR patients might stay for a few days.
What is the difference in pain level post-surgery between PKR and TKR?
PKR generally results in less postoperative pain compared to TKR, as it is less invasive and preserves more of the knee’s natural structures.
How is the decision made between choosing a PKR and a TKR?
The decision is based on the extent of the arthritis, patient’s activity levels, overall knee condition, and personal health goals. This decision is made after thorough discussions with your orthopedic surgeon and after evaluating all diagnostic imaging.
How do I care for my knee after surgery?
Post-surgery knee care involves managing pain, preventing infection, attending physical therapy, and gradually increasing activity levels under the guidance of your healthcare provider.
What are the signs of complications after knee replacement surgery?
Signs to watch for include excessive swelling, redness, pain that worsens over time, any discharge from the incision site, fever, or any sudden decrease in mobility.
Can a PKR be converted to a TKR if needed in the future?
Yes, if arthritis develops in the other compartments of the knee, a PKR can be converted to a TKR. This is a common scenario and can be effectively managed with surgery.
What are the latest advancements in knee replacement surgery?
Recent advancements include the use of robotic-assisted surgery for greater precision, improvements in implant materials for increased longevity, and less invasive surgical techniques that aid in faster recovery.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
