Case Study: Management of Quadriceps
Rupture in a 66-year-old Female
The patient is a 66 yr old female, with complaints of the right leg, knee pain for the past 1 week. The patient was at a shopping mall when she sustained a fall from the escalator. The patient was taken to the emergency room where an X-rays were taken and she was splinted. She is currently taking Ibuprofen for pain.
The pain is associated with swelling, bruising, tingling, numbness, radiating pain, weakness, gait. The problem has been getting worse since it started. Walking, standing, lifting, exercise, twisting, lying in bed, bending, squatting, kneeling, stairs, sitting make the symptoms worse. Rest, ice, lying down makes the symptoms better.
The patient is a diabetic on Metformin and glipizide. She is also taking Lipitor for hyperlipidemia and Atenolol for hypertension. She has a surgical history of hysterectomy and laparoscopic cholecystectomy.
Upon examination of the right knee, there is tenderness to palpation along the distal aspect of the quadriceps tendon. Effusion is present. The patient has a palpable gap at the proximal aspect of the patella. The patient cannot tolerate McMurray’s maneuvers or stability testing due to discomfort and swelling. The knee lacks a full range of motion secondary to pain.
The patient cannot perform a straight leg raise and have a weakness with extension. Clinically patella baja is present. Neurovascularly is intact distally. There are no erythema, warmth, or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
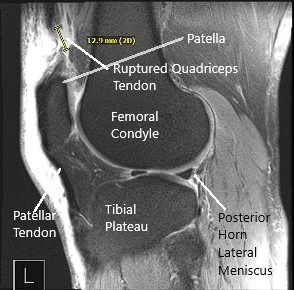
He was diagnosed with quadriceps rupture clinically. MRI of the right knee was performed and suggested a full-thickness rupture of the distal quadriceps tendon occurring 1.8 cm proximal to the patellar insertion site and resulting in a tear gap measuring up to 1.5 cm
All treatment options including surgical and nonsurgical were discussed with the patient at length. Risks, benefits, and alternatives were also discussed with the patient. The patient agreed to go ahead with the surgical procedure.
PREOPERATIVE DIAGNOSIS: Quadriceps rupture, right thigh.
POSTOPERATIVE DIAGNOSIS: Quadriceps rupture, right thigh.
OPERATION: Quadriceps repair through transosseous tunnels, right knee.
DESCRIPTION OF THE PROCEDURE: The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced and he was intubated.
The right lower extremity was prepped and draped in a usual aseptic fashion after tourniquet was applied over the upper thigh. Time-out was called. Esmarch was used to exsanguinate the extremity.
A midline vertical incision was given centering over the superior pole of the patella to expose the distal quadriceps as well as the distal pole of the patella. A complete tear of the quadriceps tendon was found.
The joint was exposed. The serosanguineous fluid was drained and the knee joint was washed thoroughly. The debridement of loose muscle and periosteal tissue was done.
The superior pole of the patella was exposed and the pole was denuded and decorticated to prepare a bed for insertion of quadriceps. Three transosseous tunnels were made from the superior pole to the inferior pole and the suture passer was used to pass back sutures through the three tunnels.
Now, the quadriceps tendon was prepped and two #5 FiberWire were used to pass Krackow stitch on either side, 5 locking knot each limb, or either suture. The sutures were passed into the patella through 3 transosseous tunnels. The two central limbs were identified on either side and passed off to the side of their respective sutures.
The knee was put in full extension and the sutures were knotted on the inferior pole of the patella. The medial and lateral extensor retinaculum was repaired using 0 Vicryl. 30 degrees of flexion of the knee did not cause any tension on the sutures and the repair.
The wound was again washed and closure of the wound was performed in layers using Vicryl #0 and Vicryl #2-0 followed by Monocryl #3-0 pull-out sutures. Steri-Strips were applied and the dressing was done. Tourniquet was released. The patient was extubated and moved to the postoperative recovery unit in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
