The patient is a 48-year-old female who works as a gym instructor and presents with a complaint of right shoulder pain. The patient reports she is unable to extend her arm forward and experiences severe pain during overhead activities. The patient denies any recent trauma but believes repetitive movements of the shoulder during her 20-year long job lead to her symptoms.
The patient describes the pain as stabbing. The pain is intermittent and does disturb her sleep. The pain is however not associated with any tingling, numbness, radiation, weakness, bowel or bladder abnormality. Activities such as lifting and ones that require overhead movement of the arm make the symptoms worse. The patient states that icing makes her symptoms better.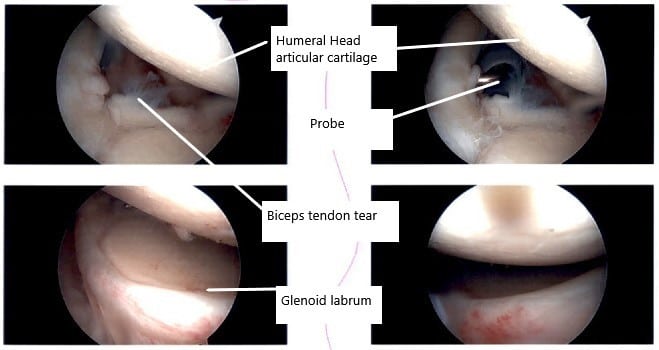
Intraoperative arthroscopic images of the shoulder joint.
The patient’s past surgical history is significant for lumbar fusion surgery and laparoscopic hernia repair. The patient has no medical history. The patient has no allergies and denies the use of any illicit drugs. The patient quit smoking 5 years ago. The patient had previously tried various conservative measures such as physical therapy, cortisone injections, and pain medications but without any significant relief.
On examination of the right shoulder, the patient sits with the scapula protracted and depressed. They are tenderness to palpation over the anterior supraspinatus and proximal biceps. There is mild palpable crepitus in the subacromial space with ranging.
The patient has a restricted range of motion at the last 20 degrees of overhead abduction and discomfort with the above shoulder range of motion. The patient has discomfort with impingement maneuvers Whipple testing. The shoulder is stable on the exam. They have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth, or skin lesions present.
Forward Flexion (Normal – 180 degrees) – 160 degrees
Extension (Normal – 50 degrees) – 50 degrees
Abduction (Normal – 180 degrees) – 160 degrees
Adduction (Normal – 50 degrees) – 40 degrees
Internal Rotation: upto TL junction
External rotation: 60 degrees
On examination of the contralateral extremity, the patient is non-tender to palpation and has an excellent range of motion, stability, and strength. MRI of the right shoulder suggested acromioclavicular joint hypertrophy with capsular thickening and Joint effusion. Rotator cuff tendinopathy and fraying with 10 mm ill-defined articular tear of the supraspinatus at the mid to posterior insertion.
Abnormal morphology of the superior mid anterior labrum suggesting tear. Biceps tendinopathy and tenosynovitis with interstitial tearing of the anchor. Capsular thickening can be seen with adhesive capsulitis. Due to the failure of conservative management, the patient has advised surgical management. After discussion of all risks, benefits, and potential complications, the patient agreed to go ahead with the surgical repair.
PREOPERATIVE DIAGNOSES: Rotator cuff tear of the right shoulder, acromioclavicular arthritis, and biceps tear of the right shoulder.
POSTOPERATIVE DIAGNOSES:
- Biceps tear, right shoulder.
- Acromioclavicular osteoarthritis.
- Bursal surface partial rotator cuff tear.
- Labral tearing, right shoulder.
OPERATIONS:
- Right shoulder arthroscopic extensive debridement.
- Right shoulder subacromial decompression and acromioplasty.
- Right shoulder distal clavicle excision.
- Right shoulder mini-open subpectoral biceps tenodesis.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where he was placed on a well-padded operating room table. General anesthesia was induced. He was turned into a left lateral position with the right shoulder up. The right shoulder was prepped and draped aseptically in the usual fashion.
He was held in a beanbag with axillary rolls in a well-padded position. All the bony prominences were well padded. A preoperative antibiotic was given. Aseptic cleaning and prepping and draping were performed in the usual fashion. Time-out was called.
The posterior entry portal for the shoulder was made through the soft spot. The scope was entered into the shoulder glenohumeral joint. An anterior entry portal was made by using a spinal needle and a small incision was given right by the coracoid process. Shaver was introduced from the anterior portal.
Examination of the shoulder showed fraying of the labrum as well as a tear of the biceps at its insertion into the labrum. Biceps tenotomy was performed. The rest of the examination was normal. There was no articular site rotator cuff tear. The scope was entered into the subacromial space where subacromial bursitis was present. Shaving was performed. Shaver was used to debriding the subacromial bursa. A lateral anterior portal was made.
The scope was entered from the lateral anterior portal and further shaving was performed on the posterior portal. Acromioplasty was performed for type 2 acromion by using the Bovie followed by a burr.
After a thorough acromioplasty was performed, the AC joint was examined and found to have arthritis. Distal clavicle excision was started from the posterior portal and then the shaver was moved into the anterior portal and the distal clavicle by about 1 cm was excised.
Pictures were taken and saved. There was a partial rotator cuff tear on the bursal side. A thorough examination was performed and it was found to be partial only. There was no deep connection to the joint. So a decision was done not to repair the rotator cuff tear.
Debridement of the rotator cuff was performed. Final pictures were taken and saved. The shoulder was irrigated and drained. Now, the shoulder was removed from the traction and put in abduction and external rotation. A 3 cm incision was given over the insertion of pectoralis major into the humerus.
Dissection was taken deep by cutting the superficial and deep fascia. The pectoralis major was seen. It was retracted laterally and Hohmann’s retractor was inserted onto the humerus. The biceps tendon was found and brought out using a right angle. A whipstitch was done into the biceps tendon.
A hole was drilled finding the biceps tendon in good tension. The whipstitch was done using Ethibond 2 and 3.5. A 4.5 mm cannulated screw with a washer was used to do the biceps tenodesis on the humerus. Excess of the tendon was cut. Final pictures were also taken.
The wound was thoroughly washed and closed in the layer using #0 Vicryl, #2-0 Vicryl, and Monocryl. The dressing was performed. Steri-Strips were put. The shoulder scope incisions were closed using nylon #3-0. The wound was thoroughly cleaned and the dressing was performed using 4 x 4, ABD, and tape.
The patient was put in a shoulder immobilizer after the surgery. The patient was awoken and sent to Recovery in a stable condition. A supraclavicular block was done before the surgery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

