The patient was a 56-year-old male, with complaints of left knee pain for the past few weeks. The patient did not recall any inciting event leading up to the onset of symptoms.
The pain was severe in intensity. The patient described the pain as aching, stabbing, throbbing, and sharp. The pain was chronic and occurred at nighttime. The problem was associated with swelling, popping/clicking, radiation, and pain with motion.
The problem had been getting worse since it started. Standing, walking, twisting, weight bearing, upstairs, downstairs, nighttime, and damp weather made the symptoms worse. The patient denied any known drug allergies.
On examination, the patient was calm, conscious, cooperative, and well oriented to time, place, and person. Upon examination of the left knee, the patient was tender to palpation along the medial joint line and had an effusion and swelling.
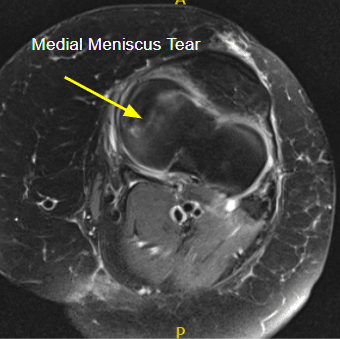
MRI of the left knee suggested radial tear of the medial meniscus and medial collateral ligament sprain/tear.
Conservative management in the form of physical therapy, medication, and exercise did not help with the pain. After discussing various treatment options, risks, and benefits of surgical and nonsurgical treatments, the patient opted for surgical management in the form of arthroscopic surgery.
The patient was informed of the possible need for a knee replacement in the future. The patient was also informed of the other risks and complications including infection, bleeding, injury to small nerves and vessels, need for rehabilitation, development of arthritis, systemic complications including blood clots, cardiac arrest or pulmonary complications, and neurovascular complications including death.
The post operative and rehabilitation protocol were discussed, and the patient consented. The informed consent was signed.
The patient was taken to the operating room and placed on a well-padded operating table. General anesthesia was induced. A tourniquet was applied. A time-out was called. The left leg was prepped and draped aseptically.
A lateral anterior entry portal was made and the arthroscopy was inserted. A medial anterior portal was made using a spinal needle. Examination of the medial tibial compartment showed a radius tear of the posterior body of the posterior horn of the medial meniscus. Resection of the margins of the tear was performed with the use of biters and shavers which achieved balanced margins.
There was also a horizontal tear which was debrided. Balanced margins would be achieved. There was Grade III to Grave IV osteoarthritis of the medial femoral condyle. Examination of the infrapatellar notch showed an intact ACL.
Examination of the lateral femoral compartment showed intact meniscus and cartilage of the lateral tibiofemoral compartment. Examination of the patellofemoral compartment showed Grade I to Grade II tear of the cartilage of the patella which was debrided with the use of a shaver.
Final arthroscopic pictures were taken. The knee was lavaged with copious normal saline. The wound was closed using nylon #3-0. The dressing was done using Xeroform 4 x 8s, ABD, Webril, and ACE wrap.
The patient was extubated and moved to the recovery room in a stable condition.
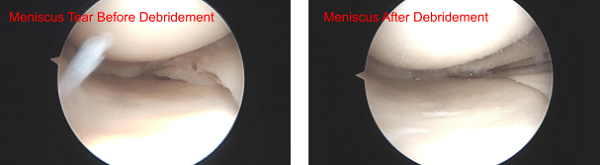
Meniscus before and after Debridement
The patient followed up in office regularly and started with physical therapy and a home exercise program for the rehabilitation of the knee. Ice and elevation was used to reduce pain and swelling. The patient followed up in the office and recovered completely in 8 weeks.

