Case Study: Selective Nerve Root Block in
a 70-year-old Female with Radiculopathy
A 70-year-old patient was in our office, with complaints of pain radiating to the right leg for the past 2 months. The pain was extremely severe in intensity, described as 8 on a scale of 0 – 10. The patient describes the pain as stabbing. The pain was intermittent and does disturb sleep. The pain was associated with radiation and limping.
The pain was not associated with swelling, bruising, tingling, numbness, weakness, bowel or bladder abnormality, giving way. The problem has been getting unchanged since it started. The patient has a prior surgical history of a right meniscal repair and right carpal tunnel release. The patient has a medical history of sarcoidosis, hypertension, and high cholesterol.
The patient was currently taking Motrin for pain, lisinopril, and metoprolol for hypertension and pravastatin for hyperlipidemia. The patient did not smoke. The patient did have allergies. The patient was working as a music teacher but describes an increasing difficulty in carrying her daily activities and job due to pain.
On general examination, the patient was calm, conscious, cooperative, and well oriented to time place and person. Upon examination of the lumbar spine, the patient was tender to palpation over the right paraspinal musculature. There was no tenderness over the spinous processes and there was no evidence of crepitus with ranging. The range of motion of the spine was limited due to discomfort.
The straight leg raise test was positive. There was no tenderness on palpation over the trochanteric bursa and hip. There was no soft tissue swelling and ecchymosis. The patient has a full range of motion of the hips. The hips are stable on the examination.
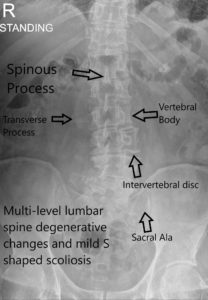
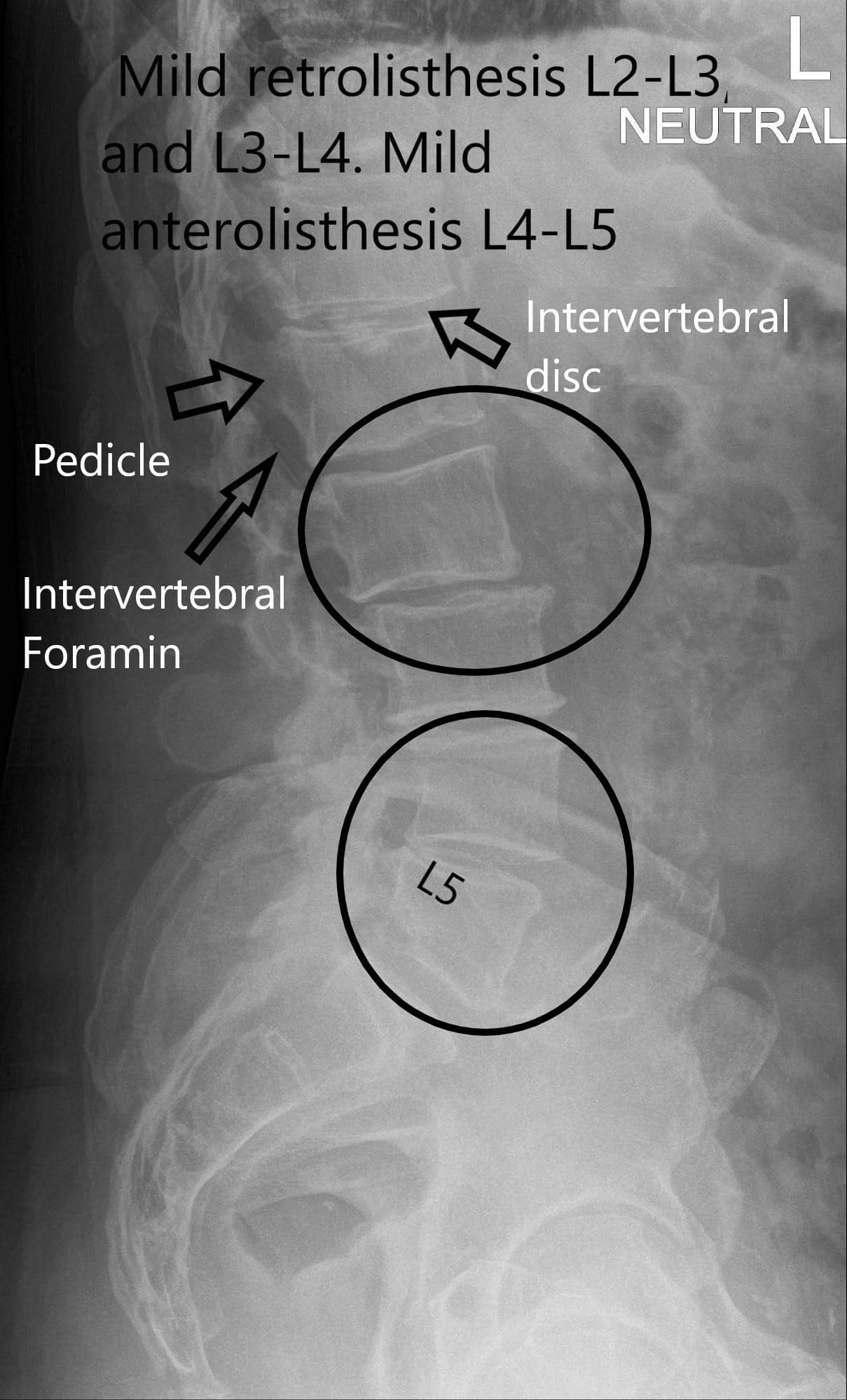
The strength was 5/5 in bilateral lower extremities and there was no distal neurovascular deficit. There are no erythema, warmth, or skin lesions present. The examination of bilateral upper extremities revealed no neurovascular deficit. The Babinski reflex was indeterminate bilaterally, Hoffman’s sign was negative and Lhermit’s sign was negative. X-ray Lumbar Spine suggested multilevel lumbar degenerative changes, mild retrolisthesis L2-L3, and L3-L4. There was mild anterolisthesis L4-L5.
X-ray LS Spine AP view.
X-ray Lateral view of LS spine.
The patient had radiculopathy of the right L5, degenerative disc disease, and Spondylolisthesis L4-5 with degenerative scoliosis. Treatment options discussed with the patient at length. The patient was advised to keep precautions along with heat and ice therapy. Options such as selective lumbar nerve block discussed with a patient and an MRI are requested.
MRI suggested mild thoracolumbar levoscoliosis. Mild retrolisthesis at L2-L3. Spondylosis and facet arthrosis. Small left far lateral disc protrusion at L2-L3, with minimal contact on the left L2 nerve. Moderate right paracentral disc protrusion at L4-L5, encroaching mildly on the right L5 nerve root. Mild central canal stenosis at L3-L4. Mild-to-moderate central canal stenosis at L4-L5.
MRI of the lumbar spine.
Physical therapy and Medrol Dosepak was prescribed. The Medrol Dosepak helped transiently. Various treatment options were discussed and the patient opted for nerve root block. The risks and complications including temporary or permanent injury to the nerve root, worsening of pain, vascular embolization of the medication after effects, among others. The patient understood and signed informed consent.
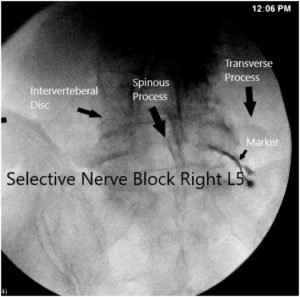
The patient was taken to the procedure room where she was laid prone on the operating table. The area of interest was prepped and draped aseptically in the usual fashion. A C-arm was brought in and the entry portal was marked with the C-arm squaring the LS-S1 disc space. Local anesthesia of Xylocaine 1% 3 ml was used to infiltrate the area of entry.
A #22 gauge spinal needle 5 Inches was Introduced after the time-out was introduced along with the access of the C-arm. Once the needle hit the bone, it was brought inferiorly and final images were checked in AP and lateral views and found to be in the adequate place. A right L5 neurogram was produced in a satisfactory fashion. The picture was taken and saved.
Intraoperative fluoroscopic image.
The area was infiltrated using 0.5 ccs of 1% Marcaine and 40 mg of Kenalog. The needle was removed and a Band-Aid was applied. The procedure was uneventful. The patient was moved to the recovery unit in a stable condition.
Patient had excellent relief after the nerve block. The relief lasted for 3 months. Patient had the procedure repeated once more and had excellent relief since then for the last 1 year.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.