Case Study: Kyphoplasty for Wedge Collapse of
L1 Vertebrae in a 62-year-old Female
A 62-year-old female presented to our office with complaints of lower back pain for the past 5 months. She allegedly had a fall from height (11 feet) while working at home. She was diagnosed with a compression fracture of the L1 vertebrae and prescribed medications along with a Taylor brace.
The patient states the pain has been constant and although the pain medications provided some relief initially, they have been not effective recently. The pain is described as a dull to sharp ache in the back that is rated as severe in intensity. The patient reports disturbed sleep secondary to pain.
The pain is not associated with tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or limping, hand function difficulty. Activities such as walking, standing, lifting, exercise, twisting, lying in bed, bending, stairs, sitting make the symptoms worse. Rest, ice, lying down, makes the symptoms better.
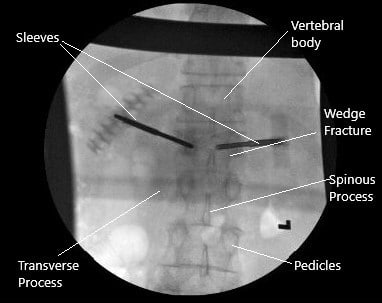
Intraoperative X-ray of the kyphoplasty.
The patient works in a medical office and is currently not working. Her past medical history is significant for coronary artery disease and hypertension. Both conditions are currently stable on medications. She is a nonsmoker and drinks alcohol socially. She denies any known drug allergies.
On physical examination, bony palpation elicited tenderness of the spinous process at L1. There were positive thump and rotational tenderness. Active range of motion: lateral flexion to the left (20 deg.) and the right (20 deg.); rotation to the left (20 deg.) and the right (20 deg.); and flexion (30 deg.), extension (10 deg.), and pain with motion.
Passive range of motion: lateral flexion to the left (20 deg.) and the right (20 deg.); rotation to the left (20 deg.) and the right (20 deg.); and flexion (30 deg.), extension (10 deg.), and pain with motion.
Motor Strength: L1-2 Motor Strength on the Left: hip flexion iliopsoas 5/5. L2-L4 Motor Strength on the Left: knee extension quadriceps 5/5. L5 Motor Strength on the Left: ankle dorsiflexion tibialis anterior 5/5 and great toe extension extensor hallucis longus 5/5. S1 Motor Strength on the Left: plantarflexion gastrocnemius 5/5.
Neurological System: Babinski Reflex Left: plantar reflex absent. Sensation on the Left: T12 normal, L1 normal, L2 normal, L3 normal, L4 normal, L5 normal, S1 normal, S2 normal, and normal distal extremities.

Intraoperative fluoroscopic image of kyphoplasty.
Due to failure of conservative management in the form of Taylor brace and pain which was worsening without any activity, kyphoplasty was advised to the patient. The risks and complications of the surgery including infection, bleeding, injury to nerves and vessels, leakage of cement, need for open surgery among others were discussed at length with the patient. The patient understood and signed the informed consent.
PREOPERATIVE DIAGNOSIS: Wedge collapse of L1 vertebra.
POSTOPERATIVE DIAGNOSIS: Wedge collapse of L1 vertebra.
OPERATION:
- Kyphoplasty of the L1 vertebra through bilateral pedicles.
- Bone biopsy.
- Use of fluoroscopy
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where general anesthesia was induced. He was turned prone on Jackson’s table with Wilson’s frame. All bony prominences were well padded. The area was marked and cordoned. The surgical area was prepped and draped aseptically in the usual fashion. Preop antibiotics were given. Time-out was called.
C-arm was brought in and the L1 vertebra was localized in the AP and lateral view. The pedicles of the L1 vertebra were localized on both sides. A spinal needle was used to make an entry through the facet joint into the pedicle. Bilateral entries were made to the lateral pedicles.
Once the Jamshidi needles were on the medial pedicle, the lateral view was checked and they were found to be in a satisfactory position. The Jamshidi needles were advanced further. A bone biopsy was taken from the medial vertebrae and sent for histopathology.
Once we found the Jamshidi needles in appropriate position, the Jamshidi needles were removed. The sleeves were withdrawn by about a centimeter and balloons were inserted on both sides. The balloons were inflated. We felt that there was a breach on the inferior endplate on the right side, so the inflation was stopped at that time.
Bone cement was mixed and inserted on right and left sides. About 4 ccs of cement could be inserted. There was a suspected breach of the inferior endplate, but the cement was still in the vertebral body. The tamps were put into the sleeves till cement was hardened. The sleeves were removed. The final picture was taken in the AP and lateral view and saved. The wound was thoroughly washed.
The closure was done using #2-0 Vicryl and #3-0 Monocryl. The dressing was done using Dermabond, Steri-Strips, and Tegaderm. The patient was turned to supine and moved to Recovery in a stable condition after extubation. Postop examination of the patient showed neuro intact. The patient had some pain in the back. The patient was able to move his both lower extremities.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
