Case Study: Management of a 57-year-old female with cervical canal stenosis, cervical compressive myelopathy, and brown sequard syndrome
The patient is a 57-year-old female presenting with complaints of worsening neck pain and weakness in the right upper and lower extremity for the past year. The patient worked as a dance instructor and is currently unable to work secondary to her symptoms.
The patient previously underwent a workup for multiple sclerosis in the form of EMG/NCS, blood tests, and lumbar puncture by her neurologist. She also had a trial of i.v steroids with no benefit. Subsequent imaging studies suggested meniscal repair and possible brown sequard syndrome.
The pain and weakness in the upper and lower extremities have been getting worse since it started. The patient stopped working and finds it difficult to navigate day-to-day activities such as climbing stairs. The patient previously had a right knee meniscal repair and right shoulder arthroscopic surgery. Her medical history is otherwise unremarkable and she denies any known drug allergies.
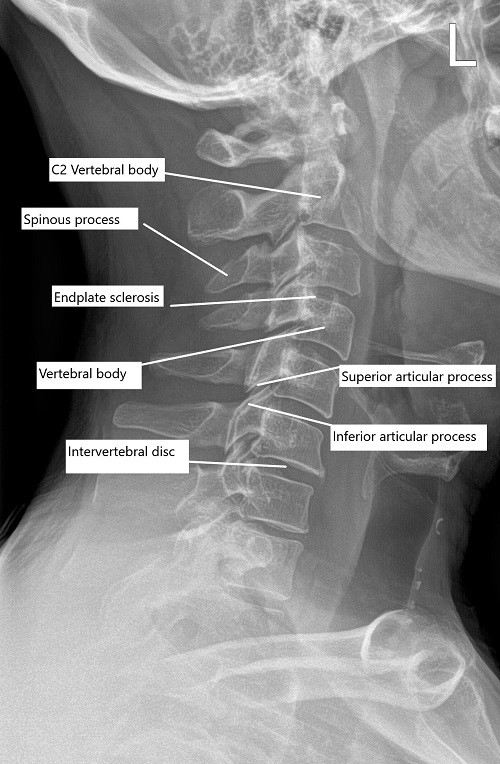
Pre-operative x-ray of the cervical spine in lateral view.
Physical examination corroborated with the imaging studies and extensive discussions were held with the patient with regards to the surgical management of the disease process. A discussion regarding disc arthroplasty versus fusion surgery at one or both levels was held with the patient. The patient has been adamantly against any fusion surgery on his neck.
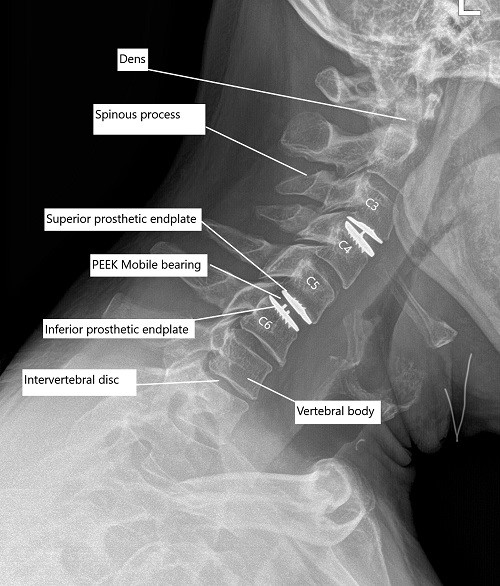
Post-op x-ray of the cervical spine showing total cervical disc replacement at C3-C4 and C5-C6 level.
The patient strongly opted for disc replacement surgery. The patient understood and wished to proceed. We discussed risks and complications including infection, bleeding, injury to vital structures and adjacent structures, neurological deterioration, CSF leak, systemic complications like cardiac, neurological, pulmonary, blindness, and even death. The patient understood and signed the informed consent.
PREOPERATIVE DIAGNOSES:
- Cervical canal stenosis, central and right side at C3-4.
- Central canal stenosis, C5-6.
- Compressive cervical myelopathy.
- Brown-Sequard syndrome with involvement of right-sided motor and left-sided sensory.
OPERATIONS:
- Anterior discectomy, bilateral foraminotomy C3-4
- Total disc arthroplasty cervical using Mobi-C 15 mm x 15 mm x 5 at C3-4.
- Anterior discectomy, bilateral foraminotomy C5-6
- Total disc arthroplasty cervical using Mobi-C 17 mm x 15 mm x 6 mm at C5-6.
DESCRIPTION OF PROCEDURE:
The patient was taken to the operating room where IV line and arterial line were secured. The patient was intubated. Neuromonitoring was put in place. Foley catheter was passed. The patient was put supine with neck extended with a shoulder roll and a doughnut under the head.
Both upper extremities were wrapped with drapes. An x-ray was done to check the level and the C-spine could be x-rayed until C6 without strapping the shoulder and so the strapping of the
shoulder was not performed. The neck was prepped and draped aseptically in the usual fashion.
A time-out was called. Preoperative antibiotics were given. A right-sided incision was given as planned. Supraplatysmal dissection was done. Platysma was cut in the line of incision using a hemostat and Bovie. Subplatysmal superior and inferior dissection was done. They were multiple dislodged veins, which were cauterized.
A plane was developed between the strap muscles and the sternocleidomastoid. The deep fascia was cut. The prevertebral fascia was reached. A hemostat was put on the midline of the cervical spine and an x-ray was done. It was found to be at the level of the C3 vertebra. The C3 disc was marked.
The prevertebral fascia was cut. Casper pins were put in C3 and C4 to achieve distraction and C3-4 discectomy was performed using Bovie, curettes, Kerrison punch 2 mm.
Posterior osteophytes were removed using Kerrison punch 1 mm and 2 mm. PLL was excised to achieve central decompression. Right- and left-sided foraminotomies were performed. There was an ossified disc on the right side, which was excised. Intraoperative Decadron was planned at the time of decompression.
Templating of the disc was performed and 15 mm x 15 mm x 5 disc replacement was planned. Templating was checked under C-arm and found to be satisfactory. Mobi-C total cervical disc 15 mm x 15 mm x 5 mm was opened and inserted.
It was checked under C-arm AP and lateral views and found to be well centered. The inserter was removed and the disc was impacted and final pictures were taken and saved.
Attention was moved to the C5-6 disc. The prevertebral fascia was cut over the C5 disc. Casper pins were reinserted in C3 and C4 to achieve distraction C5-6 discectomy was performed using Bovie, curettes, and Kerrison #2 and Kerrison #1 punches. Posterior osteophytes and PLL were excised using Kerrison #1 punch.
Burr was used to squaring the disc space. A template was used for 6 mm x 17 mm x 15 mm and found to be satisfactory. A mobi-C disc of the same size was inserted. X-rays were taken in AP and lateral views and found to be satisfactory.
The inserter was removed. The disc was finally impacted. The incision was thoroughly washed. Hemostasis was achieved. Surgifoam mixed with 40 mg of Depo-Medrol was applied to the wound.
The closure was performed in layers using #2-0 Vicryl and #4-0 Monocryl. The dressing was done using Steri-Strips. The patient was recovered from anesthesia and extubated. The patient was moved to the recovery room in stable condition. He was able to move all four extremities.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
