Case Study: Management Of A 58-Year-Old Male
With Acute Monoparesis Of The Dominant Arm
A 58-year-old male patient who comes to the emergency room, seeking care after experiencing an acute decline in his function. He states his left arm and hand just don’t work anymore and he is having numbness and tingling in his arms bilaterally.
He has a complex history of cervical spine surgeries and states that he can longer bear the pain and he is afraid because he is left hand dominant. On examination, he was extremely weak his left arm especially in his left-hand grip and wrist extensor and flexors as well as having unremitting pain that was radicular in origin over the left arm.
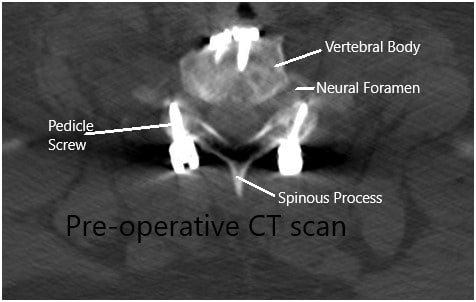
Imaging study revealed lateral disc herniations encroaching upon the neural foramen at C7-Tl and at Tl-T2, causing critical stenosis. Given his constellation of systems and weakness, we suspected also that he had a postfixed brachial plexus. obtained a thorough workup given the complexity of the patient’s imaging findings and clinical presentation and included MRI of the brain and brachial plexus.
The MRI of brachial plexus did not show any abnormalities with the brachial plexus itself, however, it did show swelling and inflammation of the nerve roots in question due to the severe amount of compression and disc fragments encroaching upon the neural foramen.
Given his a monoparesis and the fact that it was involving his dominant hand as well as the unremitting pain he was experiencing despite conservative therapy and inpatient medicines for several days in the hospital, we offered him emergent decompression. He understood all the risks, benefits, and alternatives of the surgery and gave informed consent.
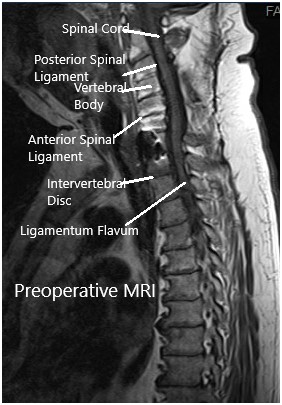
MRI suggested postoperative changes with the fusion of the facets from C3-C7 bilaterally with laminectomies. C7-T1 vertebral bodies are fused anteriorly. There is a resultant artifact as the result of the hardware.
Mild signal abnormality in the spinal cord at C5-6 of uncertain chronicity. At T1-T2 broad-based disc bulge with articular recess narrowing bilaterally. There were lateral disc herniations encroaching upon the neural foramen at C7-Tl and at Tl-T2, causing critical stenosis.
Preoperative MRI in the sagittal section.
Preoperative CT scan in the axial section.
The patient was identified in the preoperative holding area and then brought to the operating room where he was induced under general anesthesia and intubated without any issues.
Neuromonitoring electrodes were attached and tested and we attached the Mayfield head clamp and we turned the patient’s prone on to a Jackson table with chest pads. We secured the Mayfield to the Wilson frame attachment and padded all pressure points to make sure safety for the patient.
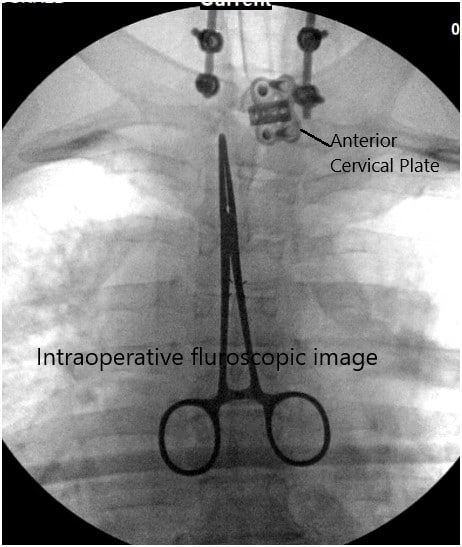
Fluoroscopy was used to localize our region of interest and then prepped and draped the patient’s cervicothoracic region. Call to order was completed and perioperative antibiotics were dosed intravenously. At this point, we made an incision with the #10 blade down to the subcutaneous fat and thereafter followed a midline avascular plane with the Bovie cautery down to the spinous processes.
There were some large veins that were cauterized during the dissection. We were able to expose the spinous processes of C7, Tl, and T2 and we followed out our dissection along the laminae exposing the transverse processes so that we could place self-retaining retractors to hold the skin muscle edges apart.
We used the McCulloch retractors to this. We then employed fluoroscopy once again to ensure our level of operation and we were able to confirm the C7 level by the visualization of previous instrumentation to that level.
We then employed a high-speed drill attached to a 3-mm matchstick burr which we used to create laminotomies and foraminotomies bilaterally at C7, Tl, and T2. We left the posterior structures intact, so the posterior tension band would remain for the patient’s stability.
Once the ligamentum flavum was exposed, we used additional drilling to expose the C8 and Tl nerve roots bilaterally. We used the combination of 1 mm and 2 mm, Kerri, on punches to do partial facetectomies and wide foraminotomies.
There was severe stenosis especially on the left side over the C8 nerve root and over the Tl nerve root. This stenosis was critical and required more drill work than on the right side to ensure a safe decompression. After the nerve roots were decompressed, we turned our attention to the hypertrophy of ligamentum flavum and resected this bilaterally using Kerrison punches.
Intraoperative fluoroscopic image.
We were able to expose the dura safely and we checked our decompression using the Woodson instruments and blunt nerve hook. The nerve roots on the side appeared very red and swollen and so we applied epidural steroid paste. We washed out the wound copiously with bacitracin irrigation and placed vancomycin powder on the field.
At that point, we disinserted the paraspinal muscles using Bovie cautery and rotated them medially until they moved over the spinous processes and used O Vicryl sutures to plicate the paraspinal muscles to cover the defect created by dissection down to the spine.
We then created a fascial advancing flap to reduce the tension of the wound and reapproximated the fascia using O Vicryl sutures in an interrupted fashion. The deep dermal layer was closed with 2-0 Vicryl sutures in an interrupted fashion followed by a running nylon stitch.
We did not insert drains and we achieved hemostasis using meticulous bipolar cautery. The patient was taken off his Mayfield head holder whereafter he was turned supine to the operating room table and extubated. All neuromonitoring signals remained stable throughout the case. The patient was shifted to the post-op ward in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.