A very pleasant patient developed neck pain and radiculopathy after a fall. They underwent extensive conservative management including Physical therapy, steroid injections, rest, and additional therapies without benefit.
They started developing arm weakness as well and increasing pain. The physical examination showed weakness in their hand muscles. Magnetic resonance imaging (MRI) of the cervical spine showed extensive neural foraminal and central canal stenosis.
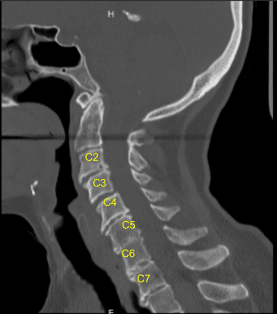
The CT scan was suggestive of Degenerative disc disease at multiple levels. The patient gave informed consent, understanding all of the risks, benefits, and alternatives to surgery. We discussed treatment options and agreed to go ahead with Anterior Cervical Discectomy and fusion C3 to C6.
The patient was identified in the Preoperative Holding Area by two separate patient identifiers and then brought back to the Operating Room where they were induced under general anesthesia and intubated without incident.
Neuromonitoring electrodes were attached and tested. The patient was placed supine on to the Operating Room table with their head in a gel doughnut and a small interscapular bump placed to position the neck in a natural lordotic position.
We localized our incision using a radiopaque marker and traced the incision with an indelible marker from the midline of the trachea to the medial border of the sternocleidomastoid muscle on the patient’s right side. We then prepped and draped the neck in the usual sterile fashion, dosed IV antibiotics, and completed a call time out.
A #15 blade was used to incise the skin along the natural skin crease and thereafter reverse Metzenbaum technique was used to create a subcutaneous dissection plane. We then undermined the platysma muscle and cut it sharply using bipolar cautery to control bleeding.
Subplatysmal dissection was carried out with mosquito hemostats and reverse Metzenbaum technique. We followed the fascial plane on the medial border of the sternocleidomastoid muscle down to the fascia anterior to the spine, and carefully retracted the esophagus and carotid artery out of view. We localized our level of operation using fluoroscopy.
We then used handheld retractors to hold the skin and muscle edges apart and deflated the endotracheal cuff to just before a cuff leak. Undermining the longissimus muscle with Bovie cautery and freeing up the disc spaces from overlying tissues, we were then able to apply our self-retaining retractor set and completed our exposure of the disc spaces from Cc to C6.
There was significant osteophytic overgrowth and we removed this bone and flattened the anterior vertebral bodies using Leksell Rongeurs and the drill. We morselized and saved this bone for use later in the case.
At this point, we placed Caspar pins into the C3 and C4 Vertebral bodies and applied gentle distraction. Using a combination of curettes, Kerrisons, rongeurs and pituitary rongeurs, we started our discectomy and applied gentle distraction as we continued our discectomy down to the posterior longitudinal ligament.
The disc was extremely degenerated at this level and we reached the posterior longitudinal ligament and undermined it and resected it using 2 mm and 3 mm Kerrison punches.
Posterior osteophytes were then removed with a drill and Kerrison punches and we created wide foraminotomies bilaterally and followed the nerve roots out through the neural foramen using the blunt nerve hook freeing them from all compressive elements and mobilizing them.

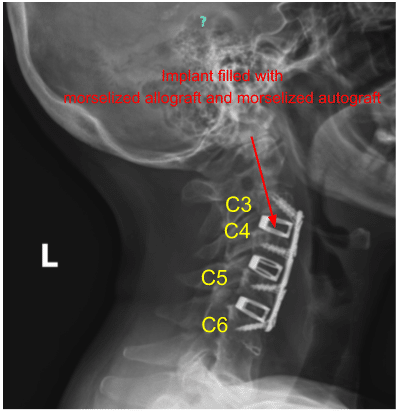
Epidural bleeding was controlled easily with Surgiflo and gentle cotton tamponade. We then trial-sized our implant and obtained x-rays. We filled our implant with a morselized allograft and morselized autograft.
We inserted it carefully under direct visualization and used x-rays to ensure appropriate placement. We then removed the inserter and washed out the wound. We thereafter removed the Caspar pin from the C3 vertebral body and covered the hole with bone wax.
We transferred our attention to the C4/C5 disc space and frame-shifted our retractors cephalad. We inserted a Caspar pin into the C5 vertebral body, applied gentle distraction, and repeated the process here for discectomy and arthrodesis.
Using a combination of curettes, Kerrisons, rongeurs and pituitary rongeurs, we started our discectomy and applied careful distraction as we continued our discectomy down to the posterior longitudinal ligament. The disc was extremely degenerated at this level.
We reached the posterior longitudinal ligament and undermined it and resected it using 2 mm and 3 mm Kerrison punches. Posterior osteophytes were then removed with a drill and Kerrison punches and we created wide foraminotomies bilaterally and followed the nerve roots out through the neural foramen using the blunt nerve hook freeing them from all compressive elements and mobilizing them.
On the right side in the neuroforamen, the uncinate joint was hyperostotic and fused to the dural, so a small cerebrospinal fluid leak was encountered. This was controlled used custom-cut gelfoam, which was carefully placed with the blunt nerve hook. We then applied a tiny amount of surgicel and fibrin glue. There was no visible leak after multiple inspections.
Epidural bleeding was controlled easily with Surgiflo and gentle cotton tamponade. We squared out the disc space with the high-speed drill and prepared the disc space for arthrodesis. We then trial-sized our implant and obtained x-rays. We filled our implant with morselized allograft and morselized autograft.
We inserted it carefully under direct visualization and used x-rays to ensure appropriate placement. We then removed the inserter and washed out the wound. We thereafter removed the Caspar pin from the C4 vertebral body and covered the hole with bone wax.
We then transferred our attention to the C5/C6 disc space and frame-shifted our retractors cephalad. We inserted a Caspar pin into the C6 vertebral body, applied gentle distraction, and repeated the process here for discectomy and arthrodesis. Using a combination of curettes, Kerrisons, rongeurs and pituitary rongeurs.
We started our discectomy and applied careful distraction as we continued our discectomy down to the posterior longitudinal ligament. The disc was extremely degenerated at this level. We reached the posterior longitudinal ligament and undermined it and resected it using 2 mm and 3 mm Kerrison punches.
Posterior osteophytes were then removed with a drill and Kerrison punches and we created wide foraminotomies bilaterally and followed the nerve roots out through the neural foramen using the blunt nerve hook freeing them from all compressive elements and mobilizing them.
Epidural bleeding was controlled easily with Surgiflo and gentle cotton tamponade. We squared out the disc space with the high-speed drill and prepared the disc space for arthrodesis. We then trial-sized our implant and obtained x-rays. We filled our implant with morselized allograft and morselized autograft.
We inserted it carefully under direct visualization and used x-rays to ensure appropriate placement. We then removed the inserter and washed out the wound. We thereafter removed the Caspar pin from the C5 and C6 vertebral bodies and covered the hole with bone wax.
At this point we spent considerable effort and time drilling down the anterior osteophytes to make a smooth surface for appropriate placement of an anterior plate.
We measured out our anterior plate, placed it over our levels of interest, and pinned it into place. We obtained x-rays, and then applied the screws as listed above. We locked all the screws in place and obtained final AP and lateral x-rays.
We then washed out the wound copiously with irrigation and used bipolar cautery to achieve meticulous hemostasis. We applied steroid paste to the retroesophageal space and closed the platysma muscle with a running #3-0 Vicryl stitch.
The platysma was reapproximated using 3-0 running Vicryl. The deep dermal layer was closed with inverted interrupted #3-0 Vicryl sutures and the skin was closed with a #5-0 running subcuticular Monocryl stitch.
The incision was dressed with Steri-Strips and the patient was placed in a cervical collar prior to being transferred off of the Operating Room table extubated. All counts were correct at the end of the case x2 and I was scrubbed for all portions of the case.
There were no changes from baseline in neuromonitoring at the end of the case. The patient was extubated in the operating room.
Patient followed up one week after the surgery and then continued to follow up 4, 6, 8, 12 and 24 weeks after the surgery.
The patient made a full recovery and continued to take part in regular daily activities. A postoperative cervical spine 2 or 3 view x-ray was ordered and the sagittal view is shown below.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
