Case Study: Anterolateral lumbar discectomy and
arthrodesis via left flank retroperitoneal approach
A patient with a past medical history of coronary artery disease and severe end-stage renal disease on three times weekly dialysis with intractable back pain, who failed nonoperative management.
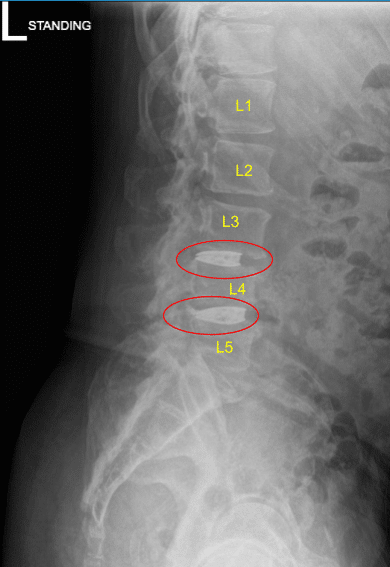
MRI and CT of his lumbar spine demonstrated severe degenerative disc space breakdown at L3-L4 and L4-L5 and accordingly they were offered a surgery for discogenic pain. The risks and potential benefits of surgery were extensively explained to the patient.
First and foremost, the risk that pain might not improve with a technically successful and complication free surgery, the risk of bleeding, infection, spinal fluid leakage, nerve injury, thecal sac injury, bowel incontinence and the rare potential risk of iliac vessel and intestinal injury were also explained to the patient.
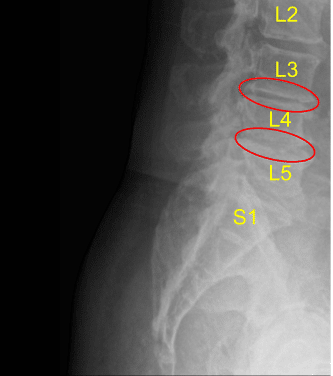
Disc space narrowing at L3-L4 and L4-L5
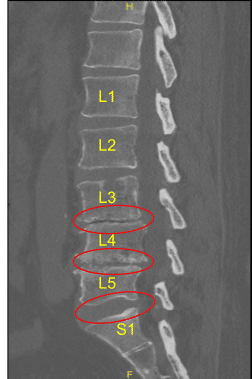
Disc bulge and facet arthropathy
They signed informed consent and were brought to the operating room for the aforementioned procedure. The findings of the preoperative lumbar spine x-ray are shown above and the patients also had a preoperative computerized tomography scan (CT scan) shown above.
The operations performed were an Anterolateral lumbar discectomy and arthrodesis via left flank retroperitoneal approach, L4-L5 anterolateral lumbar discectomy and arthrodesis via left flank retroperitoneal approach, placement of intervertebral biomechanical devices (lordotic 3d printed titanium graft) at L3-L4 and L4-L5 levels, and morselized allograft used to augment intervertebral biomechanical fusion.
The patient was identified by two separate name markers and brought into the operating room and general endotracheal anesthesia was induced. All appropriate lines were placed by the Department of Anesthesiology. Short-acting paralytics were used.
Baseline motor evoked and somatosensory evoked potentials were obtained. A twitch test was obtained showing the absence of all paralytics particularly useful for the L4-L5 level. Care was taken to monitor the patient’s femoral and saphenous nerves. The patient was positioned in the right lateral decubitus position with his left flank pointing upwards.
Their iliac crest was placed on the break of the Steris table. They were secured in place with a 3-inch silk tape in the lateral position after all pressure points had been confirmed padded. The table was jackknifed to allow his iliac crest to fall away from the L4-L5 disc space.
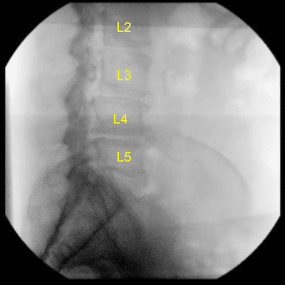
Intraoperative X-ray
AP and lateral radiographs were used to position him in a true lateral and AP position with his spinous processes equidistant from the pedicles and with his residual endplates crisp on lateral fluoroscopy. The left flank position was then carefully scrubbed, prepped and draped after two separate transverse flank incisions were marked out overlying the L3-L4 and L4-L5 disc spaces under fluoroscopy.
Gram-positive and gram-negative prophylaxis was administered. The patient was then draped in a standard neurosurgical sterile fashion. Members of the operating team went to wash their hands.
Following draping, a final time-out was carried out identifying the patient and the nature of surgery to be performed, the level of the spine to be operated on, and expected roles and responsibilities of all associated team members. Following completion
of the successful time-out, the left flank incision was infiltrated with 0.25% Marcaine with epinephrine and opened with a #10 blade to commence the case.
The case was begun at the L4-L5 level. Dissection was carried down with monopolar electrocautery to the abdominal fascia, which was opened with monopolar electrocautery in line with the skin incision. Self-retaining Weitlaner retractors were placed.
The fibers of the external and internal oblique musculature were bluntly penetrated with bimanual tonsil clamp dissection. The transversalis fascia was bluntly penetrated. A transversalis dilatation maneuver was carried out using the NuVasive MaXcess
dilatation assembly.
Stimulation was carried out and found to have no neural elements whatsoever in proximity through a transversalis dilatation. The MaXcess dilator was docked at the posterior third of L4-L5 disc space under lateral fluoroscopy and affixed in place with a K-wire.
Serial dilatation was then carried out utilizing the NuVasive MaXcess dilators. A MaXcess retractor was assembled with a blade length of 120 mm and passed over a stacked dilatator assembly in transversalis fashion.
After AP and lateral radiographs confirmed excellent positioning at the posterior third of the L4-L5 vertebral body, the MaXcess retractor was affixed in place with the articulating arm and the interior of the MaXcess retractor was carefully inspected with visual confirmation of no neural elements within the blades.
Stimulation was carried out with an electrophysiologic ball-tip probe. Once we were certain that there were no neural elements within our MaXcess retractor, it was affixed in place at L4-L5 disc space with a shim blade and opened in a craniocaudal and anteroposterior fashion. Time-out was started and the remainder of this case was carried out with care being taken to keep overall retraction time under 15 minutes.
The disc was incised with a bayoneted annulotomy knife and aggressively resected with Cobb elevators. Serial dilatational maneuvers were carried out with bullet type trials so as to fully indirectly decompress the L4-L5 disc space and the exiting L4 nerve roots.
No residual disc was found. Some small fragments of cartilage were resected utilizing pituitary rongeurs. This corresponded with the preoperative vacuum disc phenomenon seen on CT scan. The end-plates were meticulously maintained intact and scraped bare with a ring curette.
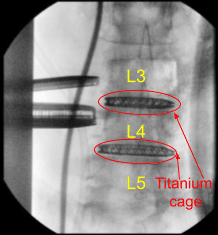
Once we were certain that the disc space was prepared for arthrodesis, an 8 x 55 x 22 mm lordotic 3D printed titanium cage was selected from the NuVasive tray and impacted into place at the L4-L5 disc space. Excellent indirect decompression and completion of L4 neuroplasty was seen with separation of the L4 and L5 vertebral bodies.
Once the cage had been inserted to the appropriate depth spanning the entirety of the L4-L5 disc space, it was released from the cage inserter. The area was inspected one final time, copiously irrigated with antibiotic impregnated saline, and the MaXcess retractor blade was then collapsed. The shim was removed and the retractor was removed to allow the fibers of the psoas musculature to fall inwards.
Postoperative X-ray
Attention was then turned to the L3-L4 disc space. Exactly the same procedures that had been carried out at L4-L5 was carried out at L3-L4 beginning with an incision overlying L3-L4 through the epidermis using a #10 blade, followed by dissection down to level of the abdominal fascia using monopolar electrocautery for hemostasis.
A self-retaining Weitlaner retractor was placed. The fibers of the abdominal fascia were divided with monopolar electrocautery. Bimanual tonsil clamp dissection was utilized to separate the fibers of the external and internal oblique down to the level of the transversalis fascia. Transversalis fascia was bluntly penetrated with tonsil clamps and an identical transversalis dilatation at L4-L5 was carried out with the MaXcess retractor.
Once the dilators had been affixed to the L3-L4 disc space at the posterior aspect with the K-wire and stimulation was carried out ensuring no neural element surrounding this, the MaXcess retractor with the blade length maintained at 120 mm was passed over a stacked dilator assembly and following identical inspection of the L3-L4 disc space with visualization.
The retractor was affixed in place with a shim blade following electrophysiologic stimulation ensuring no neural elements were within our field of view and was opened in a craniocaudal and anteroposterior fashion.
The disc was incised with an annulotomy knife at L3-L4 and then aggressively resected using Cobb elevators to separate the cartilaginous endplates followed by pituitary rongeurs. Once again, the majority of the disc was found to be completely degenerated and collapsed. Some small fragments were sent to Pathology.
Serial bullet trials were impacted into the L3-L4 disc space to complete an indirect decompression and neuroplasty of the exiting L3 nerve roots. The bony endplates were then aggressively prepared with a ring curette following withdrawal of the bullet paddles. An 8 x 50 x 22 mm lordotic CoRoent titanium cage from the NuVasive tray was then directly impacted into L3-L4 disc space to complete the arthrodesis.
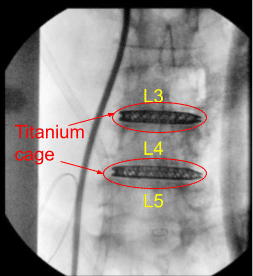
Intraoperative X-ray
AP and lateral radiographs indicated excellent cage positioning, restoration of lordosis, and indirect decompression throughout. Accordingly, the L3-L4 cage was released from the cage inserter. The area was copiously irrigated with antibiotic impregnated saline and packed with Surgiflo hemostatic matrix product.
The shim blade was then removed. The MaXcess retractor blades were collapsed and the retractor was withdrawn with direct visual inspection of the psoas musculature. No suggestion of psoas hematoma was seen whatsoever.
Accordingly, the case was felt completed with a two-level anterolateral interbody fusion being performed very efficiently at the L3-L4 and L4-L5 levels. The abdominal fascia was reapproximated with interrupted figure-of-eight #0 Vicryl sutures followed
by layered subcutaneous skin closure with inverted interrupted #2-0 Vicryl sutures followed by a running subcuticular #4-0 Monocryl suture to reapproximate both skin edges.
At the close of the case, the patient’s bed was taken out of jackknife position and the patient was positioned supine. No changes in motor evoked and somatosensory evoked potentials were noted throughout. The patient was then extubated uneventfully following reversal of general endotracheal anesthesia.
They were found to be in the same condition in which they entered the operating room, which is to say awake, alert, following commands briskly with full motor powers in his upper and lower extremities. They had no complaints of radicular pain at rest.
The patient followed up in two weeks after the surgery and showed signs of improvement. The patient also then continued to follow up in 4, 6, 8, 12, 24 weeks. In their last office visit the patient stated they were able to do their usual activities.
Postoperative X-ray Sagittal View
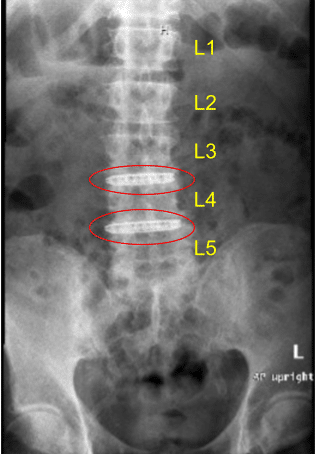
Postoperative X-ray

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
