Case Study: Left L4-5 Laminoforaminotomy, Microdiscectomy
The patient had been seen by us multiple times in our office for radicular pain with tingling and numbness over the thigh and leg on the left side for the last year. The patient reported that the quality of the pain was aching and sharp.
The pain would be aggravated by factors such as going up and downstairs, lifting, pushing or pulling, standing, and walking. We had discussed and tried non operative treatment which failed. Recently, They had started to feel it on the right thigh as well.
They had magnetic resonance Imaging (MRi) done which showed degenerative disc disease with kyphosis of the lumbar spine along with disc herniation of left L4-5. The images are shown below.
We discussed treatment options including minimal invasive microdiscectomy versus fusion surgeries of the lumbar spine. The patient opted for limited surgical treatment, which included microdiscectomy. We discussed risks and benefits including infection, bleeding, injury to nerves and vessels, failure, need for rehab, need for repeat surgery, and need for fusion surgery in the future among others.
We discussed the complications including blood clot, cardiac, pulmonary or neurological complications among others. The patient understood and signed the informed consent. After this assessment the plan was to move forward with a Left L4-L5 Laminotomy, discectomy. The diagnosis was lumbar radiculopathy.
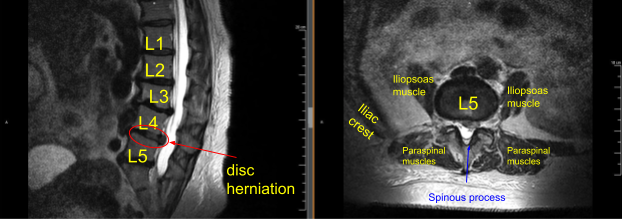
Sagittal View Axial View
The patient was taken to the operating room where general anesthesia was induced. Neuromonitoring was put in place with the use of electrodes. The patient was turned prone onto a Jackson table with a Wilson frame. Her arms were put by her side in abduction and flexion. All the bony prominences were well padded.
The patient was strapped to the bed. A spinal needle was used, and fluoroscopy was done to locate the needle, which was marked. The back was prepped aseptically in usual fashion. Draping was performed. Preoperative antibiotic was given. Time-out was performed. Anesthesia was given in the area of interest of about 3 cm.
Dissection was taken deep along the tissue onto the fascia. The fascia was cut in the midline. The Cobb elevator was used to elevate the tissue off the left side of the spinous process of interest. With dissection with a Bovie, the lamina could be reached. A Woodson was inserted under the lamina for confirming the level and it was found to be under the L4 lamina. Further dissection was done and McCulloch retractors were put in.
The microscope was brought in at this time. High-speed matchstick drill bit was used to perform a laminotomy and removal of the left L4 lamina to expose the ligamentum flavum and the nerve root. Excess of bone and ligamentum flavum was removed with the use of #2 and #3 Kerrison punches.
The nerve root was seen. The nerve root was retracted medially with the use of a nerve root retractor and the disc was reached. Annulotomy of the disc was performed with a bayonet blade. Discectomy was performed thoroughly with the use of pituitaries.
The disc was explored with the use of probe as well as ball-tipped probe. Thorough discectomy was performed with the use of straight and angled micro pituitary. Irrigation was done with the use of a syringe. Hemostasis was achieved with the use of bipolar as well as epidural vein sealer (Aquamantys). A Penfield probe was inserted into the disc space and a final picture was taken and confirmed that we were at the L4-5 level.
The wound was thoroughly irrigated and drained. Surgiflo was put to achieve hemostasis. This was drained. 80 mg of Depo-Medrol was injected in the nerve roots. This was followed by achieving hemostasis and closure of the fascia. Exparel was injected into the paravertebral muscle as well as the subcutaneous tissue.
Closure was done in layers using 0 Vicryl for the fascia, 2-0 Vicryl for the subcutaneous and 4-0 Monocryl. Dermabond was used to seal the skin followed by Telfa and Tegaderm. The patient was turned prone onto the bed and extubated. Post Op neurological status was intact. The patient was moved to recovery in stable condition. The neuromonitoring did not show any changes, rather there was improvement in the left L5 nerve root after the decompression.
The patient followed up one week after the surgery and then continued following up in our office 4, 6, 8, 12, weeks after surgery. In their last office visit the patient’s showed improvements in posture and radicular pain with tingling and numbness. The patient will follow up again in 6 months.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
