Case Study: Management of 73-year-old Female
with Cervical Spine Stenosis and Myelopathy
A 73-year-old female with a history of alcoholism, COPD, BPH, aspiration pneumonia, tobacco abuse, and peripheral neuropathy was sent from a rehabilitation Center with complaints of upper extremity weakness, urinary incontinence, decreased sensation to upper and lower extremities.
She was seen in the hospital where she was found to be profoundly weak in her upper extremities and her lower extremities had numbness and tingling. His imaging studies showed critical stenosis from C3 to C6.
She was currently on gabapentin, latanoprost, pantoprazole, atorvastatin, tiotropium bromide, and tramadol. The patient was an active smoker. She had no known drug allergies.
CT of the cervical spine demonstrated multilevel posterior disc bulges with bilateral neural foraminal stenosis of the mid to lower cervical spine. Sclerotic hypertrophic degenerative changes were associated with the mid to lower cervical facets.
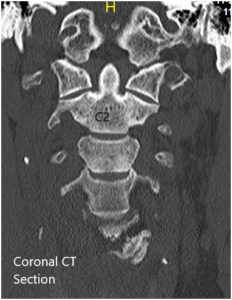
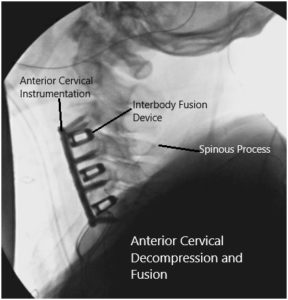
Preoperative Coronal and Axial CT sections.
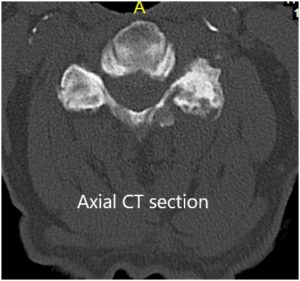
An MRI of the cervical spine suggested At C3-4, there is a central disc herniation with severe spinal canal stenosis and moderate compression of the cervical spinal cord, with compressive myelopathy. Disc protrusions are identified at C4-5 and C5-6 with moderate narrowing of the thecal sac and mild flattening/compression of the ventral cervical spinal cord. Mild narrowing of the thecal sac at C2-3 and C6-7, with a small central protrusion at C2-3.
Preoperative MRI in sagittal section.
Given the alarming imaging findings and his profound weakness that was fast progressing, we considered this neurosurgical emergency and offered her immediate decompression and stabilization. She understood all of the risks, benefits, and alternatives to surgery and we had her medically optimized as quickly as possible so that we could address her surgical issues. She gave informed consent.
The patient was identified in the preoperative holding area by two separate patient identifiers and then brought back to the operating room where she was induced under general anesthesia and intubated without any extension of her neck.
She was placed prone onto the operating room table with a slight interscapular bump on her head secured in a gel donut. His arms were tucked to the sides and x-rays were completed to ensure proper visualization of the cervical spine and anatomic positioning. Neuromonitoring was set up.
At this point, we used a radiopaque marker to localize our incision and centered on the C3-C6 vertebral bodies. We drew our incision with an indelible marker from the midline of the trachea to the medial border of the sternocleidomastoid muscle at the level of the skin following the natural crease.
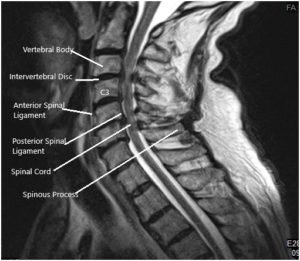
Intraoperative fluoroscopic images.
At this point, we prepped and draped the neck in the usual sterile fashion and completed a call to order. Perioperative antibiotics were given.
A #15 blade was used to incise the skin down to the level of the subcutaneous fat and thereafter combination of bipolar cautery and Bovie cautery was used to continue the dissection down to the fascia of the platysma muscle. Subcutaneous dissection was carried out and then the platysma muscle was undermined and cut with the Metzenbaum scissors.
Bleeding was controlled with bipolar cautery and subplatysmal dissection was carried out in a similar fashion. The medial border of the sternocleidomastoid muscle was identified and using blunt finger and Kittner dissection, we continued our dissection down to the prevertebral fascia.
Using handheld Cloward retractors, we exposed the prevertebral fascia identifying the carotid artery laterally both by palpation and visualization of the trachea and esophagus medially. These were held and protected out of the way and the endotracheal cuff was deflated to adjust for a cuff leak.
We cut the prevertebral fascia with Metzenbaum scissors and inserted a spinal needle to identify our level of operation using fluoroscopy. We then measured and placed our Trimline self-retaining retractor set and inserted Caspar pins into the C5 and C6 vertebral bodies.
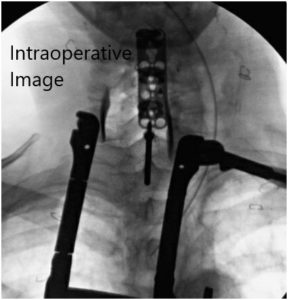
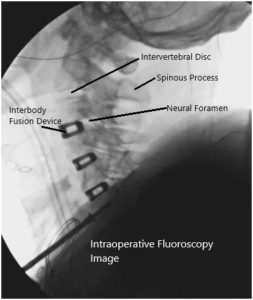
Intraoperative fluoroscopic images.
We continued our dissection using Bovie cautery freeing the longus colli muscles from the vertebral bodies and exposing the disc spaces from C3 to C6. Starting at the C5-C6 level, we incised the anterior annulus of the disc space and started our discectomy to the posterior longitudinal ligament. We applied slight distraction with the Caspar pins and used a combination of curettes, pituitary rongeurs, and Kerrison to complete our discectomy.
We used the 3 mm matchstick drill bit to clear osteophyte from our dissection field both anteriorly and posteriorly and then we undermined the posterior longitudinal ligament with a blunt nerve hook. We then resected the posterior longitudinal ligament with 1 mm and 2 mm Kerrison punches and removed additional osteophytes with 2 mm and 3 mm Kerrison punches.
We created wide foraminotomies with a 2 mm Kerrison punch and followed the nerve roots out of their foramen using the blunt nerve hook freeing them from all compressive elements circumferentially. We then prepared the endplates for arthrodesis using the curettes and the drill and controlled the epidural bleeding with Surgifoam and gentle cotton tamponade.
We then trialed sized our C5-C6 disc space and took x-rays. Once we are happy with the size of this trial, we collected morselized autograft from the drilling of the bone, and then we brought in our spacer cage measuring 7 mm in height with built-in lordosis.
We filled this interbody spacer with a combination of demineralized bone matrix, and morselized autograft. We inserted this into the C5-C6 disc space and then washed it out copiously with bacitracin irrigation.
We then shifted our attention to the C4-C5 disc space and placed a Caspar pin at the C4 vertebral body and repeated the same process for the discectomy and foraminotomies. At this disc space, there was slightly more significant osteophytic bony overgrowth, which was removed with a drill and Kerrison punches.
The posterior longitudinal ligament was resected in its entirety and we were again able to fit a 7 mm spacer into the disc space with built-in lordosis. We filled this with morselized autograft obtained from the drill and Kerrison punches as well as Trinity ELITE and DBX paste.
We then removed the Caspar pins from the C6 vertebral body and placed it into the C3 vertebral body and frame-shifted our retractors up to the C3-C4 disc space, where we repeated the process for the discectomy and the foraminotomies.
Arthrodesis was once again achieved as with the level below using the drill and curettes as well as morselized autograft and allograft placed into a sustained spacer, which was trial sized and then the final spacer was placed. At this point, we washed out the wound copiously with bacitracin irrigation and measured our cervical plate.
We applied lordosis using the handheld lordotic bender to the plate and using fluoroscopy to ensure the appropriate sizing of the plate. The cervical plate was placed anteriorly and 4.2 x 16 mm screws were then used in the C3, C4, C5, and C6 vertebral bodies. We obtained fluoroscopy throughout to ensure proper trajectory for the screws.
Once we were satisfied with the screw placements and the positioning of the intervertebral spacers, we washed out the wound copiously with bacitracin irrigation and created hemostasis using meticulous bipolar cautery.
The wound was checked for inadvertent bleeding and any and all bleeders were controlled with bipolar cautery. We applied some Surgifoam to the wound and then closed the incision in layers using #3-0 Vicryl sutures in the platysma.
Deep dermal sutures were then placed using #3-0 Vicryl sutures in the inverted, interrupted fashion followed by #5-0 Monocryl suture in the subcuticular fashion at the level of the skin. A cervical collar was placed to the patient after the dressing was applied and the patient was extubated in stable condition.
Patient was transferred to rehabilitation center after a brief hospitalization where she had a gradual uneventful recovery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
