Spondylolisthesis
Spondylolisthesis is the forward translation of one vertebra over the one below it. The condition is commonly encountered in the lower spine and may lead to a wide range of symptoms from low back pain to paralysis of the lower extremities.
Spondylolisthesis is often found in the younger age group secondary to sports or developmental disorders or in the elderly population secondary to degenerative changes. Most cases of spondylolisthesis benefit from nonoperative conservative treatments and only a small subset of patients may require surgery.
The spinal column is made of 24 small bones known as vertebrae stacked upon each other to provide a safe conduit for the spinal cord and the spinal nerves. An intervertebral disk is present in between vertebrae and functions to absorb the forces acting on the spine and to provide flexibility for movement.
Each vertebra forms four joints known as facet joints, two with the vertebra above and two with the vertebra below. The vertebral body connects with the facet joints through a bony part known as pars interarticularis.
Spondylolisthesis Causes & Pathophysiology
There may be a developmental abnormality in the structures of the vertebra making them more susceptible to stress fracture of the pars-interarticularis and subsequent spondylolisthesis. The slip may not be present at birth but may present during periods of rapid growth during adolescence as the normal soft tissue restraints give away.
The disease may also run in the family and maybe present by birth. Certain other congenital syndromes/diseases such as spina bifida may lead to spondylolisthesis.
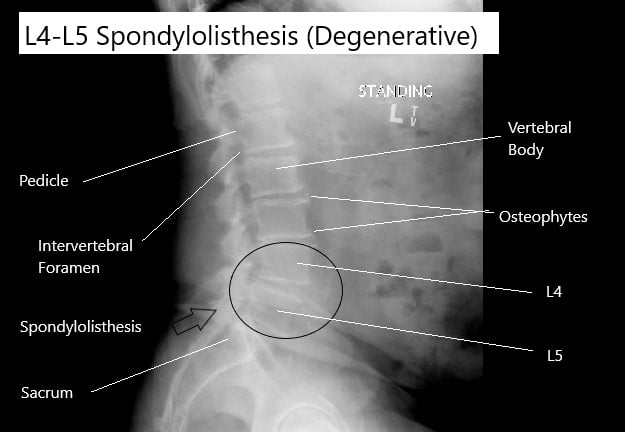
Degenerative spondylolisthesis is more common among elderly patients and mostly affects the L4-L5 level. With advancing age the intervertebral disc loses the water content and fluidity. This leads to a decreased disc height and instability of the vertebrae. The micro instability leads to facet joint degeneration and eventual slippage of the vertebrae. The body tries to realign by hypertrophy and the formation of bone spurs.
Isthmic spondylolysis is the fracture of the pars interarticularis that may cause spondylolisthesis. Stress fracture of the pars may occur in a patient participating in sports involving repetitive twisting, turning, and extension of the spine such as track and field, football, weight-lifting, gymnastics, etc. The spine level mostly involved in the isthmic type of spondylolisthesis is L5-S1.
Spondylolisthesis Symptoms
Most cases of developmental spondylolysis are asymptomatic. Symptoms may include insidious onset of activity-related back pain or buttock pain. In the cases of severe spondylolisthesis and compression of neural structures, there may be symptoms of hamstring tightness with knee contracture, radicular pain, bowel and bladder symptoms, and rarely cauda equina syndrome. In case of a sudden spondylolisthesis crisis, there may be symptoms of severe back pain that is aggravated by extension and relieved with rest.
Degenerative spondylolisthesis commonly presents with symptoms of mechanical back pain. There may be symptoms of neurogenic claudication, that presents with buttock or leg discomfort while walking upright and is relieved on sitting. There may be symptoms of radiculopathy and rarely cauda equina syndrome.
Isthmic spondylolisthesis most frequently presents as axial low back pain. There may be radiculopathy symptoms of pain traveling down the legs and neurogenic claudication. Rarely there may be symptoms of cauda equina syndrome which manifests as loss of bowel bladder control and weakness/numbness of the lower extremities.
Spondylolisthesis Diagnosis
The diagnosis of spondylolisthesis involves an orthopaedic spine surgeon extracting a thorough history of the events leading up to the symptoms. The physician conducts a detailed physical examination and tests for the integrity of the nervous system.
Radiological tests are done to diagnose the spondylolisthesis and grade the degree of slippage. Special views may be required to correctly diagnose and stage the degree of spondylolisthesis.
A bone scan may be used to diagnose stress fractures of the pars interarticularis. The bone scan may be followed by a CT scan to confirm a stress fracture or a sudden fracture of the pars interarticularis. MRI imaging usually aids in the diagnosis of compression of neurological structures and all the soft tissue structures.
Management
The management of developmental spondylolysis depends upon the severity. In asymptomatic patients and patients with only mild to moderate grade of spondylolysis only conservative management is advised. The conservative management consists of rest, physiotherapy and avoiding contact sports. Rigid bracing may be used in acute episodes.
Operative management is reserved for grade 3 and 4 spondylolysis. Patients with neurological symptoms and in patients who have persistent symptoms despite a trial of conservative are also candidates for surgical management.
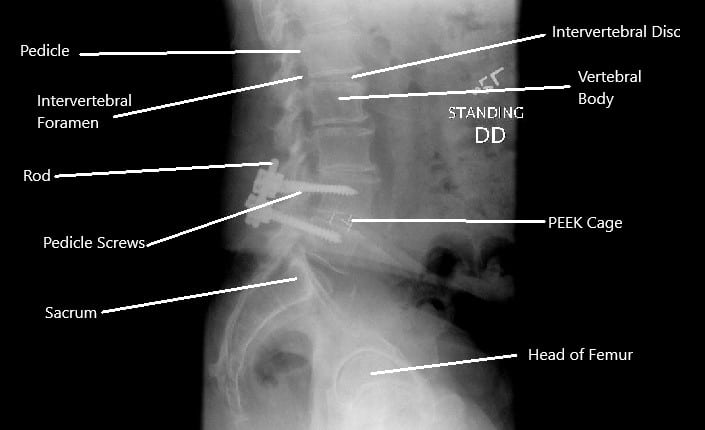
The surgical management may consist of repair of the pars interarticularis with screws, hooks or wires. Posterolateral fusion may be used in low grade with symptoms. In rare cases, a totally displaced vertebrae may be removed (vertebrectomy).
In the case of isthmic spondylolisthesis, bracing may be done in acute episodes along with conservative management. The degenerative spondylolisthesis is also initially managed with conservative treatment which may also involve use of epidural injections apart from physical therapy and pain medications.
The operative management is done in the case of isthmic and degenerative spondylolisthesis if there are persistent symptoms deposited 6-9 months of conservative management. The operative management may include decompression alone or decompression with fusion and deformity correction.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.