Sacroiliac Joint Dysfunction & Fusion Surgery
Overview
The sacroiliac joint is formed between the pelvic bones and the lower part of the spine known as the sacrum. The sacrum consists of five sacral vertebrae joined together to form a single bone. The two iliac bones of the pelvis form a joint with the sacrum, one on each side of the body. The Sacroiliac joint is responsible for connecting the lower extremities with the pelvis to the spine. The unique position of the sacroiliac joint cushions the impact of day to day activities.
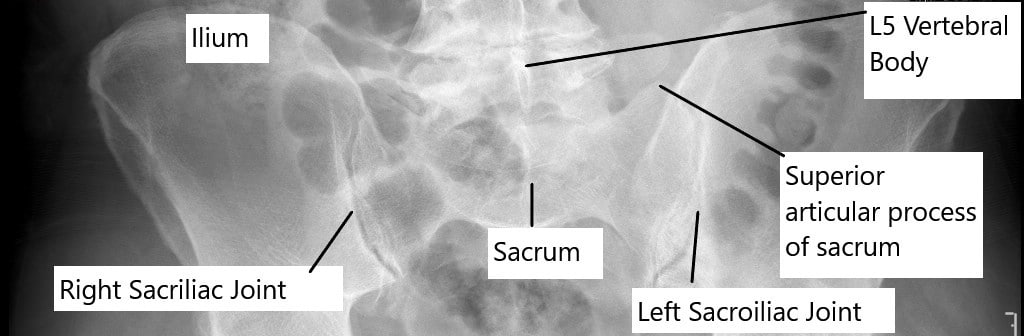
Bilateral sacroiliac joints as seen on X-ray of the pelvis in anteroposterior view.
Sacroiliac joint dysfunction is a degenerative condition of the SI joint which may frequently result in lower back pain. The location of the pain is also the site of referral of pain from other spine pathologies. The pain from SI dysfunction however stays below the lower back. The pain may also radiate down the legs to the foot. Patients may often report alleviation of symptoms when wearing a tight belt.
Although minimal, the sacroiliac joint has movement in various planes such as gliding, rotation, tilting, translation, and nodding. These complex movements are aided with help of a large group of muscles and strong ligaments attached to the joint. However, the joint motion decreases progressively with age and the joint may be naturally fused in the elderly population.
The cause of SI dysfunction is generally a result of repetitive trauma to the joint. The repetitive motion may cause wear and tear of the structures in the joint causing pain. The joint is the primary pathology in inflammatory diseases such as ankylosing spondylitis and Reiter disease.
The joint is may also be involved due to systemic diseases such as gout, hyperparathyroidism, acromegaly, or renal failure. A prior lower back spinal fusion surgery or any trauma/injury to the SI joint may also lead to SI joint dysfunction. Rarely infections and tumors may cause SI joint dysfunction.
Diagnosis of SI Joint Dysfunction
Diagnosing SI joint dysfunction can be challenging due to the overlapping symptoms with other conditions such as lumbar disc herniation or hip joint disorders. A thorough clinical evaluation is essential, including a detailed history, physical examination, and imaging studies.
Physical Examination: The physician will perform specific maneuvers to provoke pain in the SI joint, such as the FABER test (Flexion, Abduction, and External Rotation) and the Gaenslen test. A positive response to these tests can suggest SI joint dysfunction.
Imaging Studies: While X-rays, MRI, and CT scans can help rule out other conditions, they are not always definitive for diagnosing SI joint dysfunction. However, they can show degenerative changes or inflammation in the SI joint.
Diagnostic Injections: To confirm the diagnosis, a physician may perform a diagnostic injection of a local anesthetic into the SI joint under imaging guidance. If the injection significantly reduces pain, it confirms that the SI joint is the source of the pain.
Treatment Options for SI Joint Dysfunction
Treatment for SI joint dysfunction typically begins with conservative measures. The goal is to reduce pain, improve function, and prevent further joint damage.
Conservative Treatments
Physical Therapy: A physical therapist can design a program to strengthen the muscles around the SI joint, improve flexibility, and correct posture. Exercises that target the core, pelvic floor, and lower back muscles are particularly beneficial.
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation and pain in the SI joint. In some cases, stronger pain medications or muscle relaxants may be prescribed.
SI Joint Injections: Corticosteroid injections into the SI joint can provide temporary relief by reducing inflammation. These injections are often guided by imaging to ensure accuracy.
Pelvic Belts: For patients with hypermobility or instability in the SI joint, a pelvic belt may help stabilize the joint and reduce pain, particularly during pregnancy.
Interventional Treatments
If conservative treatments fail to provide adequate relief, interventional procedures may be considered:
Radiofrequency Ablation (RFA): RFA uses heat to destroy the nerves that transmit pain signals from the SI joint. This procedure can provide long-term relief for patients with chronic SI joint pain.
SI Joint Fusion: For patients with severe, refractory SI joint dysfunction, surgical fusion of the joint may be necessary. This procedure involves permanently joining the bones of the SI joint to eliminate motion and reduce pain.
Understanding SI Joint Fusion
SI joint fusion is a surgical procedure that stabilizes the joint by fusing the sacrum and iliac bones. This is typically considered when other treatments have failed to alleviate pain and improve function.
Indications for SI Joint Fusion:
- Chronic SI joint pain that has not responded to conservative treatments
- Significant joint instability or hypermobility
- Degenerative changes that severely affect joint function
Surgical Techniques:
- Open SI Joint Fusion: Involves a larger incision and direct visualization of the joint. This approach allows for more precise placement of graft material but comes with a longer recovery time.
- Minimally Invasive SI Joint Fusion: This technique uses smaller incisions and specialized instruments to access and fuse the joint. It typically results in less postoperative pain and a faster recovery.
Recovery and Outcomes:
- Recovery from SI joint fusion can take several months, during which time patients will gradually return to normal activities.
- Physical therapy is often recommended postoperatively to strengthen the surrounding muscles and improve overall function.
- While SI joint fusion can significantly reduce pain, it also eliminates joint movement, which may affect mobility in the lower back and pelvis.
Surgery is reserved for patients in whom, conservative management has failed to resolve symptoms. Sacroiliac joint fusion surgery involves the use of small triangular-shaped implants through the SI joint to stabilize and fuse the joint.
The surgery may be performed through minimally invasive techniques utilizing only small incisions to achieve the goal. The majority of patients achieve excellent stability following the surgery and experience relief from low back pain.
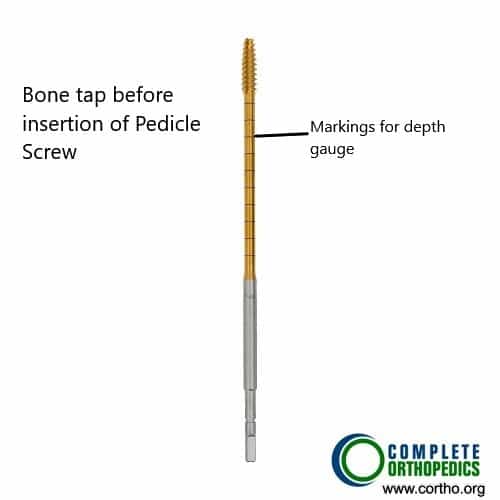
Bone tap
The bone is used for creating the path for the screw to engage in the bone. The bone tap has markings used to limit the depth of insertion during surgery.

Instruments used in posterior sacral fusion
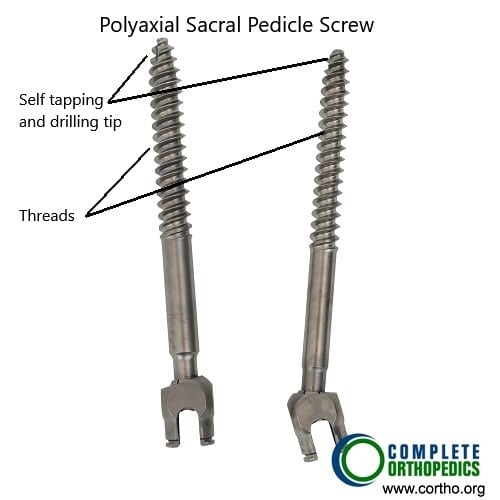
Poly-axial sacral pedicle screws
The pedicle screws with the help of instruments shown above are used in sacral fusion and with the lumbar vertebra and the iliac bone to achieve stabilization at the sacroiliac and the L5-S1 joint.
Conclusion
SI joint dysfunction is a complex condition that requires a comprehensive approach to diagnosis and treatment. Understanding the anatomy and function of the SI joint, recognizing the symptoms, and exploring the full range of treatment options, including SI joint fusion, can empower patients to make informed decisions about their care.
For patients experiencing chronic lower back pain that may be related to SI joint dysfunction, it is essential to seek evaluation by a healthcare professional experienced in diagnosing and treating this condition. With the right treatment plan, many patients can achieve significant pain relief and improved quality of life.
Do you have more questions?
What are the most common causes of sacroiliac joint dysfunction?
Common causes include trauma (like falls or car accidents), degenerative conditions like osteoarthritis, pregnancy (due to hormonal changes and increased joint laxity), inflammatory conditions (like ankylosing spondylitis), and previous spinal surgeries that alter the biomechanics of the joint.
How can I tell if my lower back pain is due to SI joint dysfunction?
SI joint dysfunction often causes pain in the lower back, buttocks, and sometimes the legs. The pain is typically on one side and worsens with activities like sitting, standing, or walking. Specific tests performed by a doctor, like the FABER or Gaenslen test, can help identify SI joint pain.
Can SI joint dysfunction resolve on its own, or does it always require treatment?
In some cases, mild SI joint dysfunction may resolve with rest, activity modification, and over-the-counter pain medications. However, persistent or severe cases typically require medical intervention, such as physical therapy, injections, or in some cases, surgery.
What are the main differences between SI joint dysfunction and sciatica?
SI joint dysfunction pain is usually localized to the lower back and buttocks, potentially radiating down the leg but not past the knee. Sciatica, however, involves nerve compression in the spine and causes pain that radiates down the leg to the foot, often accompanied by tingling or numbness.
What types of exercises are recommended for SI joint dysfunction?
Exercises that strengthen the core, improve flexibility, and stabilize the pelvic region are beneficial. This includes stretching the iliopsoas and piriformis muscles, strengthening the gluteal muscles, and performing gentle yoga or Pilates exercises designed for lower back stability.
How effective is physical therapy for treating SI joint dysfunction?
Physical therapy is highly effective for many patients with SI joint dysfunction. A well-structured program focusing on strengthening the core, pelvic floor, and stabilizing muscles around the joint can reduce pain and improve function significantly.
Are there any specific activities I should avoid if I have SI joint dysfunction?
Avoid activities that place excessive strain on the lower back and pelvis, such as heavy lifting, high-impact sports, prolonged sitting or standing, and twisting motions. It’s also advisable to avoid uneven surfaces when walking or running.
What is the role of injections in treating SI joint dysfunction?
Injections, particularly corticosteroids, can reduce inflammation and provide pain relief in the SI joint. These are often used when other conservative treatments have failed. Diagnostic injections can also confirm if the SI joint is the source of pain.
How long does the relief from SI joint injections typically last?
The relief from SI joint injections varies; some patients experience relief for several weeks to months, while others may only get temporary relief. The effectiveness can depend on the underlying cause of the dysfunction and the severity of the condition.
When should I consider SI joint fusion surgery?
SI joint fusion is considered when conservative treatments, such as physical therapy, injections, and medications, have not provided sufficient relief, and the pain significantly impacts daily activities. It’s typically a last resort for chronic, severe cases.
What is radiofrequency ablation, and how does it help with SI joint pain?
Radiofrequency ablation (RFA) is a procedure that uses heat generated by radio waves to disrupt nerve signals transmitting pain from the SI joint. It can provide long-term relief for patients who haven’t responded well to other treatments.
What are the risks associated with SI joint fusion surgery?
Risks include infection, nerve damage, blood clots, and complications from anesthesia. There’s also the potential for continued pain if the surgery doesn’t fully resolve the dysfunction. Recovery can take several months, and there may be limitations on activity during this time.
What is the recovery process like after SI joint fusion?
Recovery involves a period of limited activity to allow the joint to heal, followed by physical therapy to restore strength and mobility. Full recovery can take several months, during which patients gradually return to normal activities.
How successful is SI joint fusion in relieving pain?
SI joint fusion has a high success rate in relieving pain for patients with confirmed SI joint dysfunction, with many patients experiencing significant or complete pain relief. Success depends on accurate diagnosis and appropriate surgical technique.
Will I be able to return to normal activities after SI joint fusion surgery?
Most patients can return to their normal activities, including work and exercise, after completing their recovery and rehabilitation. However, high-impact activities may need to be modified to avoid placing excessive stress on the fused joint.
Is there anything I can do to prevent SI joint dysfunction from recurring?
Maintaining a healthy weight, staying active with regular exercise, practicing good posture, and avoiding activities that strain the lower back and pelvis can help prevent recurrence. Strengthening the core and pelvic muscles is particularly important.
Can SI joint dysfunction be misdiagnosed as another condition?
Yes, SI joint dysfunction can be misdiagnosed as lumbar spine issues, hip problems, or sciatica because the symptoms often overlap. Accurate diagnosis requires a thorough evaluation by a healthcare professional, including specific tests and possibly imaging studies.
Are there any long-term consequences of untreated SI joint dysfunction?
If left untreated, SI joint dysfunction can lead to chronic pain, decreased mobility, and compensatory issues in other parts of the spine or hips. It may also contribute to degenerative changes in the joint, worsening the condition over time.
If left untreated, SI joint dysfunction can lead to chronic pain, decreased mobility, and compensatory issues in other parts of the spine or hips. It may also contribute to degenerative changes in the joint, worsening the condition over time.
Pregnancy increases SI joint mobility due to hormonal changes that relax the ligaments. This, combined with the additional weight and altered posture, can lead to SI joint pain. Treatments include wearing a pelvic support belt, physical therapy, and modifying activities to reduce strain.
Can weight loss improve symptoms of SI joint dysfunction?
Yes, losing excess weight can reduce the strain on the SI joint, potentially improving symptoms and reducing the risk of further joint degeneration. A healthy diet combined with regular exercise can be beneficial.
Is SI joint dysfunction common in athletes, and what sports are most likely to cause it?
SI joint dysfunction is relatively common in athletes, particularly in sports that involve repetitive or asymmetric loading, such as running, gymnastics, soccer, and football. Proper training, conditioning, and technique are crucial to prevent injury.
Can lifestyle changes alone be enough to manage SI joint dysfunction?
In mild cases, lifestyle changes such as improving posture, regular exercise, avoiding triggers, and maintaining a healthy weight may be sufficient to manage SI joint dysfunction. However, more severe cases often require additional medical treatments.
What should I expect during my first consultation for SI joint dysfunction?
During your first consultation, the specialist will take a detailed medical history, perform a physical examination, and may order imaging tests. They will discuss your symptoms, potential causes, and treatment options tailored to your condition.
How can I find the right specialist to treat my SI joint dysfunction?
Look for a healthcare provider who specializes in musculoskeletal conditions, such as an orthopedic surgeon or a pain management specialist. It’s important to find someone with experience in diagnosing and treating SI joint dysfunction specifically.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
