Case Study: T6 to T11 Instrumented Fusion
A patient presented to the outpatient clinic with signs and symptoms of multiple previous spinal surgeries and a fractured left-sided thoracic rod with pseudarthrosis and surgery was recommended to stabilize his thoracic ppine.
The risks, benefits, alternatives and potential complications were explained to him. All of his questions were answered until no further issues were raised and they provided written informed consent which was placed in the chart.
The physical examination showed tenderness of the paraspinal region at L5 on the left and right side. Fractured left-sided thoracic Z-rod with pseudoarthrosis and laterally placed proximal pedicle screw. Ct study conducted prior to the surgery supported the preoperative diagnosis of thoracic pseudoarthrosis.
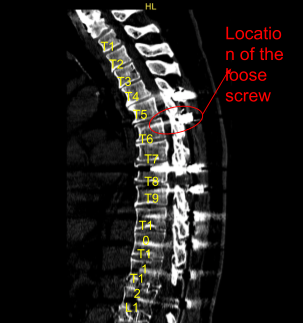
Sagittal View of Preoperative CT-Scan
The patient was brought to the operating room. Their identity was verified. General anesthesia was induced. The patient was intubated by the anesthesia service. Respiratory and cardiac monitoring leads were placed.
Neuromonitoring leads for motor evoked potentials, somatosensory evoked potentials and EMG were placed and baseline signals were obtained. The Patient was positioned prone on a Jackson Relton-Hall frame. All pressure points were carefully padded. The thoracolumbar area was cleaned with chlorhexidine.
Previous incision was demarcated. Skin was sterilized with DuraPrep solution. Sterile drapes were placed in usual manner. They received prophylactic preoperative antibiotics through IV as well as dexamethasone.
The thoracic part of the incision was infiltrated with 1% lidocaine and epinephrine and the skin was opened with a #10 blade scalpel. Hemostasis was obtained with bipolar electrocautery. Bovie, monopolar and Cobb elevators were used to carry the incision down to the subcutaneous tissues, incised the fascia sharply and exposed the left-sided Instrumentation.
We explored the fusion and found pseudoarthrosis, lack of bony fusion and fractured titanium Z-rod. Self-retaining retractors were placed. Setscrews were removed. Rod fragments were removed. Next, a neuronavigation array was placed in the left posterior superior iliac crest.
After infiltrating with local anesthesia, stab incisions were made with a #15 blade scalpel. Schanz pins were placed with a mallet. Neuronavigation array was fixed rigidly. The patient was draped sterilely. Intraoperative CT scan was obtained.
Next, the proximal screw on the left side at T6 was removed, which was found to be very loose, through the lateral position. Neuronavigation techniques were used to create a new trajectory for the pedicle screw more medially.
Decortication was performed with electric high-speed drill. Cannulation was performed with a navigated pedicle finder. The first path and screw placement was found to be too medial with a medial breach palpated. No CSK leak was seen in the cannulated tract and motor evoked and sensory evoked potentials were stable throughout. That screw was removed and again replaced more medially by creating a new tract.
We tapped with a 4.5 mm tap and placed a 40 x 5 mm titanium pedicle screw without difficulty. Decortication was performed from T6 down to T11 across transverse processes, rib heads and fusion mass that was present. The wound was irrigated copiously with Ancef-infused irrigation.
A new cobalt-chrome 5.5 mm Z-rod was selected, cut to proper size, connected to a domino side connector that was already in place across the tulips of the pedicle screws and secured with locking caps after some sort of bending was performed. All locking caps were final tightened with a torque and anti torque devices.
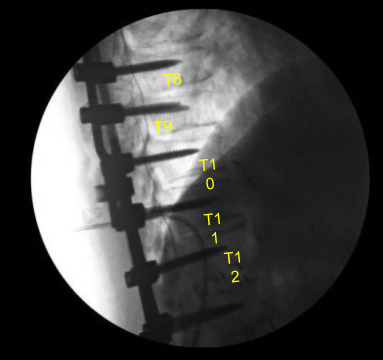
AP and lateral x-rays and final CT scan showed appropriate positioning of all the hardware. Morselized allograft with bone morphogenic protein was packed in lateral gutters on the left side for new fusion arthrodesis. Vancomycin powder was applied. Hemostasis was confirmed. A medium size Hemovac drain was tunneled in a subfascial manner and secured to the skin with a nylon suture.
Fascia was closed in a watertight fashion with interrupted 0 Vicryl Sutures. More vancomycin powder was applied. Exparel local anesthetic was then infused in the soft tissues. Subdermal layer was closed with 2-0 Vicryl sutures. The skin was reapproximated with surgical staples, cleaned, dried sterilely and dressed with a silver-impregnated bacteriostatic dressing.
Hemovac canister was applied to suction. The patient was then turned supine on the cart, extubated uneventfully and transported to the recovery room in stable condition. At the end of the case, all sponge counts, needle counts and instrument counts were correct. The patient tolerated the procedure well.
The patient initially followed up in one week after the surgery and then continued following up in our office 4, 6, 8, 12, 24 weeks. In their last office visit the patient stated they were at home and able to do their usual activities. They also stated they were doing physical therapy as well.
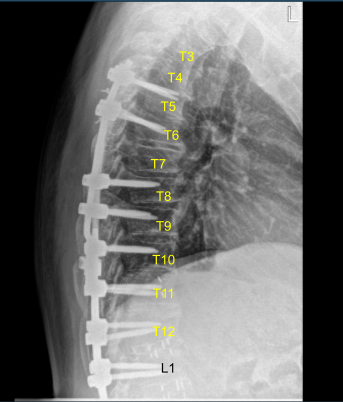
Sagittal View of Thoracic spine postoperative X-ray
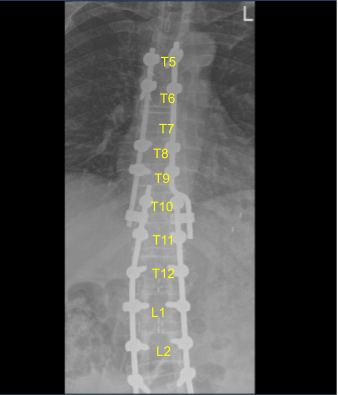
Axial view Thoracic spine postoperative X-ray
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
