Spinal Cord Stimulation
Spinal cord stimulation (SCS) is a surgical procedure used to stimulate the spinal cord and help relieve chronic back pain. The procedure is reserved for patients who have exhausted all other forms of treatment both nonoperative and operative (if indicated) to help ease the chronic back pain.
The spinal cord travels inside the conduit formed by the vertebral column starting from the base of the brain. The spinal cord travels down the body giving numerous branches known as spinal nerves and ends near the L1-L2 vertebrae. The spinal cord is responsible for sending the neural signals from the brain to all four limbs. The spinal cord also transports signals from the peripheral limbs and thorax to the brain. Together these signals help the brain to coordinate the movements of the limbs and sense the different external inputs.
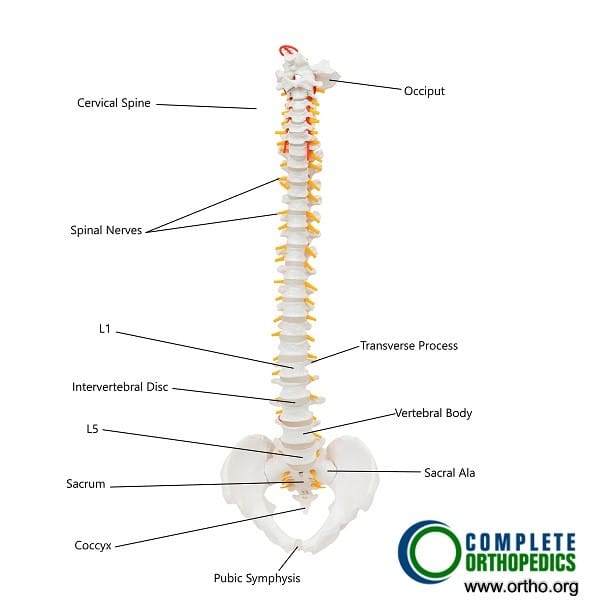
Normal anatomy of the human spine.
Pain is the body’s natural defense mechanism to help prevent further injury and usually lasts only till the inciting factor is present. The pain gradually gets better once the inciting event has subsided. The inciting event may be an infection, a tumor, a traumatic injury, or a degenerative condition. Chronic pain is usually defined as the pain that continues to affect the patient even after the inciting event is not present.
Mechanism of Spinal Cord Stimulation
The spinal cord stimulation consists of electrodes implanted under the skin that reach the space (epidural space) between the vertebrae and the covering of the spinal cord. The electrodes carry a small amount of electric current from a current generator (small device) which is also implanted in the skin. The patient has the ability to start and change the level of electrical stimulation when he experiences pain.
The stimulator does not remove the source of pain but simply alters the pain signal traveling from the spine to the brain. The altered signal does not relay the signal responsible for triggering the pain center in the brain.
Besides the basic electric impulse from the electrical generator, there are different modes depending upon the patient’s pain level and activity. The physician usually selects the mode which is best suited according to the needs of the patient.
The battery of the SCS may be non-rechargeable or rechargeable. The batteries of non-rechargeable systems may need to be changed every 2-4 years depending upon the manufacturer.
Benefits
The patients with chronic pain report a significant reduction in the intensity of the pain experienced after implantation of a spinal cord stimulator. The reduction of pain may vary among different patients but the goal is to achieve a reduction of 50% or more in the intensity of pain. With a reduction in pain, the majority of the patients report significant improvement in their quality of sleep and during their day to day activities.
Candidates for Spinal Cord Stimulation
Patients with chronic pain in whom all other forms of conservative management have failed may benefit from spinal cord stimulation. The procedure may also help patients suffering from a failed back syndrome who may not benefit from revision surgery. The patients are typically screened for any underlying psychiatric illness and drug addiction. Besides the chronic back pain caused by degenerative arthritis or trauma, patients with conditions such as complex regional pain syndrome and arachnoiditis may also benefit from SCS.
Procedure
The procedure of implanting a spinal cord stimulator first involves the implantation of a trial stimulator under local anesthesia. The trial stimulator involves the placement of an electrode through the skin to the epidural space that is connected to an external generator. The patient returns after a week or so to determine if he would get relief from a stimulator. The time period of the trial stimulator also allows the patient to report any side effects of the stimulation that may warrant not going ahead with the procedure.
The placement of a spinal cord stimulation device involves light anesthesia and the creation of holes in the vertebral structures (laminotomy) to insert the electrodes. The electrodes never touch the spinal cord directly and are placed in the epidural space (space between the vertebrae and the spinal cord lining). The wires go under the skin to attach to the generator which is implanted in the buttock.
Complications
Commonly patients may report an unusual feeling of paraesthesia upon activating the device for pain. Usually changing the frequency and intensity of transmission may alleviate the symptoms of paraesthesia. As with any surgical procedure, there may be complications of bleeding or infection. Additionally, there may be a complication of leakage of cerebrospinal fluid during the procedure causing frequent headaches.
There may be complications during the procedure such as inadvertent damage to the spinal nerves or the spinal cord from the electrodes which may cause paralysis or numbness of the extremities. There may be battery failure or skin complications from implantation of the generator and electrodes.
Conclusion
Spinal cord stimulation provides excellent pain relief in patients with chronic pain in whom all other treatment options have been tried. The device may be inserted with minimal incisions and is reversible, i.e the stimulator along with the electrodes may be taken out.
Do you have more questions?
What is spinal cord stimulation (SCS)?
Spinal Cord Stimulation (SCS) is a treatment for chronic pain where a device is implanted to deliver electrical impulses to the spinal cord, modulating pain signals before they reach the brain.
How does SCS work to relieve pain?
SCS works by interfering with the pain signals sent from the spinal cord to the brain. The electrical pulses stimulate nerve fibers, altering how the brain perceives pain, thus reducing discomfort.
Who is a good candidate for SCS?
Good candidates are patients with chronic pain that hasn’t responded to conventional treatments like medications, physical therapy, or surgery. SCS is especially effective for conditions like Failed Back Surgery Syndrome (FBSS), chronic low back pain, and Complex Regional Pain Syndrome (CRPS).
What is Failed Back Surgery Syndrome (FBSS)?
FBSS refers to persistent or recurring pain after spinal surgery. It often includes neuropathic pain that originates from damaged or irritated nerves, making SCS a potential treatment for relief.
Is SCS a cure for pain?
No, SCS does not cure pain, but it can help manage and reduce chronic pain, improving quality of life. However, it may not work for everyone, and the level of relief can vary from person to person.
How is SCS different from other pain treatments?
SCS directly targets the nervous system by modulating pain signals, unlike medications that work systemically or physical therapies that address muscles and joints. SCS also helps patients reduce reliance on medications, especially opioids.
What does the SCS trial phase involve?
The SCS trial involves temporarily placing electrodes on the spine to test if the device provides sufficient pain relief. This trial usually lasts about a week, and if successful (50% pain reduction or more), patients may opt for permanent implantation.
What are the risks of the SCS procedure?
Risks include infection, lead migration (where the electrodes move from their intended position), device malfunction, nerve damage, and the potential need for revision surgery. Approximately 4% to 31% of patients may require revision.
How long does the SCS device last?
The implanted device typically lasts 5-10 years depending on usage. Rechargeable devices tend to last longer but still need periodic replacement when the battery wears out.
Will I feel the electrical stimulation all the time?
With conventional SCS, some patients experience a tingling sensation known as paresthesia. However, newer high-frequency and burst stimulation techniques aim to provide pain relief without the tingling sensation.
How successful is SCS in reducing pain?
SCS success varies. Studies suggest that 50-70% of patients experience at least 50% reduction in pain. However, not all patients achieve the same level of pain relief, and the effectiveness may diminish over time.
Does SCS require maintenance after implantation?
Yes, patients with SCS need follow-up care to monitor the device’s function. The pulse generator may need replacement every 5-10 years, and adjustments to the device’s settings can be made as needed.
Is there a chance SCS won’t work for me?
Yes, SCS may not work for everyone. That’s why a trial phase is important, as it helps determine if SCS will provide sufficient relief before committing to a permanent implant.
Can I still take medications with SCS?
Yes, you can still take medications, but many patients find that they can reduce or eliminate the need for pain medications, especially opioids, after successful SCS therapy.
Can I undergo an MRI with an SCS implant?
Older SCS devices were not MRI-compatible, but many newer models are. However, you must always notify your healthcare provider about the implant before scheduling an MRI, as special precautions may be needed.
What types of pain respond best to SCS?
SCS is most effective for neuropathic pain (nerve-related pain), such as that experienced in FBSS or CRPS. It is less effective for pain caused by musculoskeletal issues like arthritis.
What is the difference between conventional, burst, and high-frequency stimulation?
- Conventional stimulation provides continuous electrical impulses, often leading to a tingling sensation.
- Burst stimulation delivers impulses in rapid bursts, mimicking natural nerve firing patterns, often without paresthesia.
- High-frequency stimulation uses much higher frequencies, also typically eliminating the tingling sensation.
How soon after SCS implantation will I feel pain relief?
Many patients report feeling pain relief almost immediately after the device is activated. However, some may require several adjustments to the settings before optimal pain relief is achieved.
Can SCS be removed if it doesn’t work?
Yes, if SCS does not provide adequate pain relief or causes complications, it can be removed surgically without permanent damage to your spine.
What should I expect after SCS surgery?
Post-surgery, there may be mild discomfort at the incision site. You will be asked to avoid strenuous activities while healing, and you’ll need follow-up appointments to adjust the settings and ensure proper function of the device.
Will SCS limit my physical activities?
Once fully healed, most patients can resume their normal activities. However, it’s advised to avoid high-impact sports and activities that involve significant twisting or bending of the spine, as they could affect the position of the leads.
What happens if the leads move (lead migration)?
Lead migration can cause reduced effectiveness or increased pain. If this happens, the leads may need to be repositioned surgically.
What are the long-term complications of SCS?
Long-term complications include lead migration, device failure, and loss of pain relief over time. Approximately 31% of patients may require revision surgery within 2 years due to complications like lead movement or infections
How does SCS affect my overall quality of life?
Patients who respond well to SCS often report improvements in daily activities, reduced reliance on medications, and better quality of life. However, the impact varies based on individual response to the treatment
Is SCS covered by insurance?
In most cases, SCS is covered by insurance, especially when recommended for conditions like chronic pain or FBSS. However, coverage can vary, so it’s important to check with your provider.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
