Case Study: Management of L5 Vertebral Pathological Fracture
with Collapse and Lumbar Canal Stenosis L3-S1
A 70-year-old female who presented with a chief complaint of lower back pain. She was an active person and felt something “pop” in his lower back. A couple of weeks later she fell and the following day started having back pain.
The pain has been getting progressively worse, especially while sitting in a hard chair or driving. It is relieved in the reclining position. The pain radiates down his right leg and is not associated with any numbness or tingling in his lower extremities. He wears a lumbar- support belt during the day. He denies any recent fever, bowel, or bladder changes.
The patient is in remission from rectal cancer treated with surgery, radiotherapy, and chemotherapy. Imaging was done which showed a fracture of the L5 vertebra and severe stenosis at L3/4 and LS/S1 with severe neuro-foraminal disease and degenerative changes in the spine.
The patient is calm, conscious, cooperative, and well oriented to time, place and person. Upon examination of the lumbar spine, the patient is tender to palpation over the paraspinal musculature. There is tenderness over the spinous process of L5 but has no crepitus with ranging.
There is a paravertebral muscle spasm. bilaterally around the L5 region. They have a limited range of motion of the spine due to discomfort. The straight leg raise test is positive at 60 degrees. There is no tenderness to palpation over the trochanteric bursa and hip. The patient walks with an antalgic gait.
There is no soft tissue swelling and ecchymosis. The patient has a full range of motion of the hips. The hips are stable on the examination. There is 5/5 strength in bilateral lower extremities and there is no neurovascular deficit distally. There are no erythema, warmth, or skin lesions present. The examination of bilateral upper extremities revealed no neurovascular deficit.

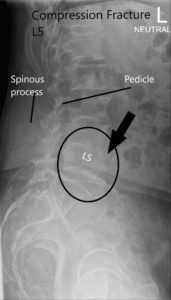
X-ray of LS spine in AP and Lateral views showing significant compression fracture L5.
The lower back pain was worsening and aggravated with sitting, standing, and moving. There was pain and numbness in the right lateral and posterior thigh (right LS-S1 radiculopathy). A CT and MRI were done as a part of the workup.
CT suggested a severe compression fracture of L5 with mild retropulsion of superior endplate. Multilevel degenerative spondylosis of the lumbar spine. Moderate to severe spinal canal stenosis at L3-L4 and L4-L5 levels.
MRI lumbar spine suggested acute or subacute compression fracture at L5. Degenerative changes with multilevel spinal canal or neural foraminal, subarticular recess stenosis were also present at L4-5 and L5-S1.

MRI showing Sagittal Section of Lumbar Sacral Spine.
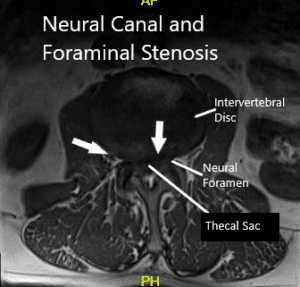
MRI showing Axial Section.
All findings were discussed with the patient, as well as treatment options. We discussed the need for biopsy to confirm the diagnosis, as it may impact his future course of treatment with regards to the malignancy.
Haemotologist and Oncologist consultations were obtained. Treatment options in the form of decompression of the spine, fixation, and fusion were discussed at length with the patient.
Management regarding open biopsy, decompression, and stabilization, its risks, complications, and recovery were discussed at length with the patient. We discussed the procedure and its risk of bleeding, infection, non-union, failure of hardware, need for repeat surgery, chances of temporary or permanent nerve or vessel injury, risk of blindness, cardiac event, stroke, paralysis, and death. We discussed the use of implants in the form of screws and rods.
The patient agreed with the plan of Decomp L3-S1, separation surgery, Pedicle screw fixation, and posterolateral fusion L4-S1 using local autograft and cancellous chips and bone allograft.
Transpedicular histopathology was sent from the left L5 body, transpedicular. The patient was taken to the operating room where generaI anesthesia was induced. A Foley catheter was passed. Needles for neurophysiological monitoring in the form of EMG, somatosensory monitoring as well as pedicle screw stimulation was done.
The patient was turned prone onto a well-padded Jackson table and positioned appropriately. The bony landmarks were all appropriately padded. The patient was secured to the operating table. The surgical area. was cordoned using 10 x 10 sticky drapes. The back was cleaned with alcohol and painted with DuraPrep. Aseptic draping was performed with Ioban.
A surgical incision was marked using bony landmarks from L3-S1. Preop antibiotic was given preoperatively. A time-out was called and the correct patient, correct procedure, and correct site were identified. The laminae of L4-S1 were reached through sharp dissection. Hemostasis was achieved. The posterior elements were exposed using Bovie on the respective sites.
The lamina of L5 was marked and a Woodson was passed into the lamina of L4 and a C-arm picture was taken to confirm our levels. After confirmation of levels. further dissection was carried out to the facet joints of L3-L4 from L4-L5 and L5-S1.
The capsules of neither of the joints were reached. Transverse processes of L4, L5 & sacral ala were exposed with dissection, and hemostasis was achieved. The lateral gutters were packed and our attention was drawn towards the laminectomy. Misonix ultrasonic bone cutter was used to perform laminectomy of L4 and L5.
Further neutral and foraminal decompression was done using Kerrison #3 and #4 for L4, L5 & S1 on both sides. Incidental durotomy (Dural tear) was found on the left side from a bone spike of L4. After decompression the durotomy was cordoned and repaired primarily using Prolene 6-0.
After achieving successful decompression from L4-S1, the inferior lamina of L3 was cut, Hypertrophic ligamentum flavum was removed using Kerrison #4. The repair was covered with a muscle patch followed by Duraseal and Surgicel in layers put to protect the dural repair.
Now the pedicle screws for the S1 were planned and the pedicle of S1 was probed from either side and checked under C-arm. After finding an acceptable position. The pedicle screw of 6 mm x 45 mm cortical fix screw was put on both pedicles of S1.
The pedicles of L5 were cannulated now and the position of the probe was checked under the C-arm and found to be acceptable and biopsy material was sucked out using a Jamshidi needle from the right pedicle of LS. Some tissue and bone marrow aspirate was sent for biopsy. A 6 mm x 40 mm cortical fix screw was inserted on both pedicles of L5.
The pedicles of L4 were cannulated similarly and checked under C-arm and found to be acceptable. A 6 mm x 45 mm cortical fix screw was inserted on both pedicles of L4. The screw heads were lined well on both sides. The wound was washed copiously with normal saline mixed with Bacitracin and gentamicin.
Decortication of transverse processes and the facets of L4–S1 were performed and the gutters were packed with a bone graft which was a mix of local autograft and allograft bone chips.
The screws were lined and rods were placed on both sides and tightened to the screw heads. The final pictures of the screw were taken with C-arm and saved. Hemostasis was achieved. Vancomycin antibiotic was sprinkled into the wound. Considering the durotomy a deep suction drain was not put. The closure was done in layers. Two suprafascial drains were put. The counts were completed, checked, and correct at the end of the procedure. The patient was transferred into a supine position on the bed, extubated, and moved to the postoperative care unit in a stable condition.
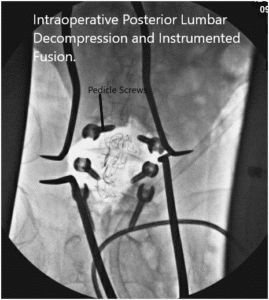
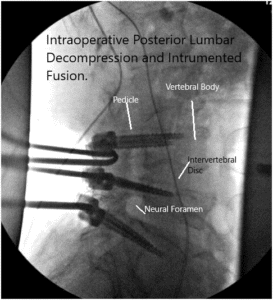
Intraoperative fluoroscopy images.


Postoperative X-ray showing AP and Lateral Views.
At six months post-op she has been living at home by himself, taking care of his dog, driving and doing activities of daily living well. He has been recovering well. He is able to walk unaided. He has been doing outpatient physical therapy. He is working out at home also. Denies headache, fever, chills, radiation, tingling, numbness, weakness.
Her pain and radiation on the right lower extremity have recovered. He plans to get more active.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
