Case Study: Management of Prolapsed Lumbar Intervertebral
Disc with Microsdiscectomy and laminotomy
The patient is a 74-year-old female presenting to us with complaints of unrelenting anterior thigh pain (right > left). The thigh pain radiated was associated with lower back pain which started 3 years ago. The patient did not remember any trauma/fall leading to pain. The patient is a retired banker and is visibly upset at her inability to carry on her day-to-day activities secondary to pain.
The patient describes the pain as sharp, stabbing, burning. The pain is constant and does disturb her sleep. The pain is associated with numbness, tingling, radiating pain, gait problem.
The pain is not associated with swelling, bruising, weakness, bowel or bladder abnormality, or limping, giving way, hand function difficulty.
The patient tried conservative therapy in the form of physical therapy and medication. She also got a cortisone injection in her back at 3 levels 3 times, every 2 weeks but the injections provided minimum relief. Activities such as standing after sitting make the symptoms worse. Rest, heat, ice, lying down, bending forwards makes the symptoms better.
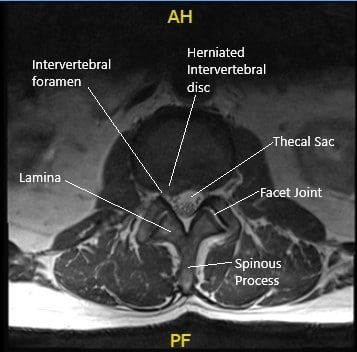
Preoperative Axial MRI section at the L2-L3 level showing herniated disc.
The patient’s past medical history is significant for hypertension, hyperlipidemia, and coronary artery disease. She is currently on atorvastatin, aspirin, and amlodipine. She denies any known drug allergies. She is a nonsmoker and has had no surgeries in the past year.
Physical examination corroborated with the imaging studies and the femoral traction test was positive. MRI imaging revealed diffuse disc bulge at L2-L3 and superimposed right paracentral disc herniation. A sequestrated disc herniation in the right lateral recess impinging the descending right L3 nerve root. There are a mild spinal canal and mild bilateral foraminal stenosis.
Various treatment options were discussed with the patient. The risks, benefits, and complications of surgery including infection, bleeding, injury to adjacent nerve and vessels, injury to the nerve root and worsening of pain, weakness, tingling, numbness, involvement of bowel and bladder, CSF leak, need for repeat surgery due to re-herniation, need for fusion in the future, systemic complications including blood clots, cardiac, neurological, pulmonary complications including death were discussed with the patient. The patient understood and signed the informed consent.
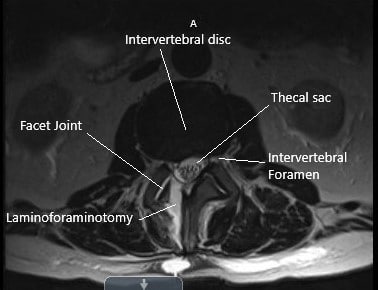
Post-operative axial MRI section showing laminoforaminotomy at L2-L3.
PREOPERATIVE DIAGNOSIS: Extruded disc of right L2-3 with right L3 radiculopathy.
POSTOPERATIVE DIAGNOSIS: Extruded disc of right L2-3 with right L3 radiculopathy.
OPERATIONS:
- Microdiscectomy of right L2-3.
- Neurolysis of right L3 nerve root.
- Laminoforaminotomy of right L2-3.
- Use of Intraoperative fluoroscopy
- Use of operative Microscope
PROCEDURE: The patient was taken to the operating room and general anesthesia was induced. The patient was flipped onto his belly over a Jackson table with a Wilson frame. All bony prominences were well padded. Her elbows were well padded. The lower back was prepped aseptically and draped in the usual fashion. A preoperative antibiotic in the form of Ancef and vancomycin was given. Time-out was called.
A spinal needle was inserted into a presumed L2 vertebral body. C-arm was brought in and lateral views were taken and confirmed that the needle was at the L2 pedicle. The skin incision was marked and the skin was incised using a #10 blade. Using Bovie deep dissection was performed through the deep fascia and on the right side of the spinous process of L2 and L3.
The lamina of L2 and L3 were exposed up to the medial facet joint. Once hemostasis was achieved, the Woodson was inserted in the L2-3 disc space and C-arm was brought in for a lateral view. The level of L2-3 was re-confirmed and saved.
A Wilson retractor was used for lateral retraction; #2-0 nylon was used for retracting the tissue on the medial side. An operating microscope was brought in and was used for further surgical management. A high-speed burr was used to remove the inferior lamina of the right L2.
Using upgoing curette and Woodson, making a plane between the ligamentum flavum and lamina, Kerrison punch #2 and #3 were used to complete the laminectomy.
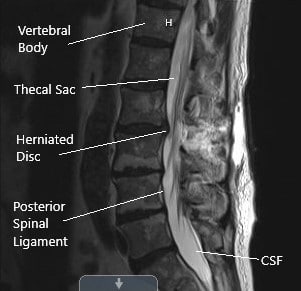
Postoperative sagittal MRI section of the lumbar spine showing laminoforaminotomy.
Further superior laminectomy of L3 was performed on the right side. The ligamentum flavum was excised to achieve central as well as lateral decompression. Woodson was used to break the adhesions over the Right L3 nerve roots. Ball tip probe was also used to dissect the nerve root laterally.
Love Nerve root retractor was used to retract the nerve roots medially and extruded disc fragments were exposed. Multiple fragments were removed using micro pituitary forceps. The disc space was sealed.
After removal of all loose fragments, irrigation of the surgical wound was performed. Far lateral decompression was checked and laminectomy and foraminotomy were completed. The right L3 nerve root was thoroughly decompressed.
Hemostasis was achieved using bipolar cautery as well as Surgiflo. After achieving satisfactory decompression, 4 ccs of Surgiflo mixed with 40mg of Depo-Medrol was injected into the surgical area and the wound was closed in layers using 0 Vicryl followed by 2-0 Vicryl and 4-0 monocryl. The dressing was performed using 4×4 and Tegaderm.
The patient was turned supine on the bed and extubated and moved to the recovery unit in stable condition. A Post-op neuro check was also performed and he was found to be intact. The patient had relief in his thigh pain, though he had pain in his back at the surgical site.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
