Back Muscle Spasms
If back pain worsens, disrupts daily activities, or is accompanied by swelling and redness, it is essential to seek advice from a healthcare professional. At Complete Orthopedics, our specialist team focuses on treating back issues with personalized treatment plans and surgical options. We emphasize understanding your symptoms, diagnosing the root causes, and recommending the most appropriate treatments or surgeries.
Our clinics are conveniently located across New York City and Long Island, and we are connected with six leading hospitals, ensuring you receive top-notch care for back problems. Schedule an appointment with one of our orthopedic surgeons either online or by phone. Discover the causes and treatments for back pain and learn when surgery might be required.
Overview
Muscle spasms in the back are defined as sudden involuntary tightness of the muscles surrounding the spine. Back spasms may affect people of all age groups and are commonly caused by certain movements/activities or underlying spine disease. Muscle spasms in the back are frequently treated with conservative therapies and rarely need surgery in case of structural spine diseases.
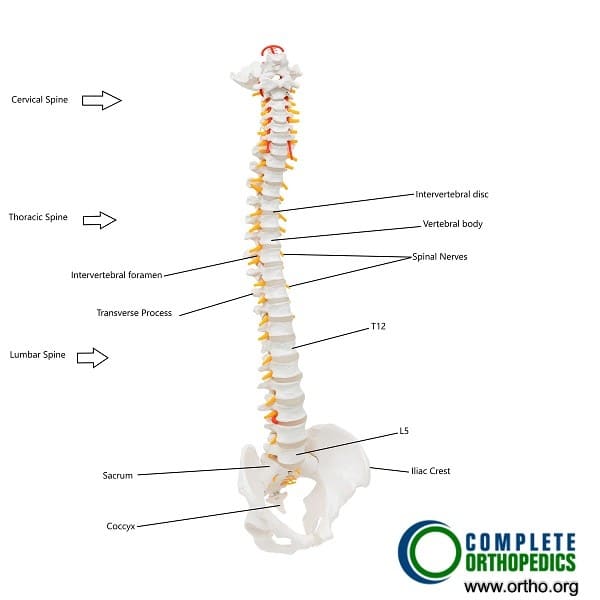
Anatomy of the Spine
Muscle groups surround the spine both in the front and the back of the spine. These muscles work together to support the spine during various movements such as bending, lifting, twisting, turning, walking, running, etc. The muscles not only aid in the movement but also provide stability to the entire spinal column. The muscle commonly involved in muscle spasms in the neck is the trapezius, and erector spinae or latissimus dorsi in the lower back.
Back Muscle Spasm Causes & Pathology
Back muscle spasms usually occur as a result of injury to the muscles involved during abnormal or repetitive activity. Patients commonly complain of muscle spasms after lifting of heavyweight, improper sleeping posture, or after sports involving repetitive spine motion. These activities may cause small tears in the muscle fibres or the tendons leading to inflammation. The involved and the surrounding muscles tighten to prevent further strain.
Excessive exercise or absence of exercise may both cause back spasms. Excessive repetitive exercise with improper technique may result in muscle strains. Similarly, inadequate exercise results in weak abdominal or back muscles which become more vulnerable to injury from day to day activities. A more serious injury such as motor vehicle accidents or a fall from a height may cause muscle spasms due to direct damage to the muscles or the structures of the spinal column.
Back spasms may also indicate an injury/disease of the structures forming the spinal column. Disk herniation, facet joint disease, spinal stenosis, degenerative disease of the spine may irritate the spinal nerves and roots leading to muscle spasms. The back muscles in the case of spinal disease tighten to act as a brace and prevent further compression/irritation of the spinal roots/nerves.
Metabolic bone diseases such as osteoporosis may lead to compression fractures of the vertebrae that may lead to subsequent muscle spasms. Inflammatory bone diseases such as ankylosing spondylitis may also cause muscle spasms.
Rarely, infection or tumors of the spinal column may also cause muscle spasms by direct irritation of the involved muscles. There may be infection or inflammation of organs such as kidneys or gallbladder leading to muscle spasms in the back.
Symptoms
The symptoms of back muscle spasms may include pain, stiffness, and tightness of the back. Pain may be worse on activities such as bending forward or lifting. Pain may be radiating in the case of an underlying pinched nerve due to spinal stenosis or herniated disk. There may be associated with numbness and tingling in the case of a pinched nerve.
Rarely in the case of cauda equina syndrome, the muscle spasms may accompany red flag signs such as loss of bladder bowel control and weakness/numbing of the lower extremities. Other red flags associated with severe spine disease are fever, weight loss, back pain at night. These symptoms require immediate medical attention and may require surgery.
Treatment
The management of back muscle spasms is generally conservative and most patients experience relief in 2-3 weeks. The physician may extract through history regarding the events preceding the symptoms and conduct a physical examination. Conservative management of muscle spasms includes using heat or cold therapy, over-the-counter medications, activity modification, and physical therapy.
Cold therapy involves icing the involved area for 10-20 mins and repeating it multiple times during the day. Cold therapy is effective in the period immediately after an injury. The cold temperature prevents further swelling/inflammation and decreases pain. The cold therapy is delivered with the help of ice-packs.
Heat therapy works by increasing the blood flow to the involved area and thereby hastening recovery. The heat also relaxes and soothes the damaged muscles, tendons, ligaments, and nerves. The heat therapy works best after 1-2 days after the injury and in chronic conditions. The heat therapy is usually delivered with the help of heating pads or warm bottles.
Pain medication such as Tylenol or Nonsteroidal Anti-inflammatory medications such as Advil/Naproxen may be used to help relieve pain and inflammation associated with muscle spasms. These medications are used cautiously in a patient with underlying conditions such as gastritis or bleeding diathesis. Sometimes, the physician may prescribe muscle relaxant medications to provide relief from severe muscle spasms.
Activity modification forms an important aspect of the management of the muscle spasms of the back. The patients are advised to avoid any activity aggravating the muscle spasms or pain. The patients are otherwise advised to remain physically active and continue day-to-day normal activities.
The majority of the patients experience significant relief with the above treatments. Patients exhibiting red flag signs such as weakness/numbness of the lower extremities and loss of bowel/bladder control may require emergency surgery to relieve the pressure off the dural sac.
The patients who fail to benefit from conservative therapy which was tried for at least 4-6 weeks may require further investigation such as an X-ray followed by an MRI to look for the pathology of the spinal column. Trigger point injections may be given to provide relief.
The management of muscle spasms due to an underlying disc herniation, spinal stenosis, metabolic bone disorder, or inflammatory spine conditions receive treatment focused on the underlying pathology. Physical therapy is usually started after the relief from symptoms. The therapy focuses on both strengthening and increasing the flexibility of the muscle in front and back of the spine.
Prevention
The prevention involves strengthening the muscles surrounding the spine and stretching the muscles to improve flexibility. The patients who are overweight or obese are advised to reduce weight. The patient is advised regarding the maintenance of proper body postures during walking, sitting, sleeping, or when engaging in sports activities.
Do you have more questions?
How long do back muscle spasms typically last?
The duration of back muscle spasms can vary. They can last from a few seconds to several minutes. In some cases, if not properly treated, they can persist for days or even weeks.
Can back muscle spasms be a sign of a more serious condition?
Yes, back muscle spasms can sometimes indicate a more serious underlying condition, such as a herniated disc, spinal stenosis, or arthritis. It’s important to seek medical evaluation if spasms are severe, recurrent, or accompanied by other symptoms like numbness or weakness.
What are the most effective home remedies for back muscle spasms?
Effective home remedies include applying heat or cold packs, taking over-the-counter pain relievers, staying hydrated, performing gentle stretches, and resting the affected muscles.
When should I see a doctor for back muscle spasms?
You should see a doctor if your back muscle spasms are severe, recurrent, or accompanied by other symptoms like numbness, tingling, or weakness. Additionally, seek medical attention if the spasms do not improve with home remedies within a few days.
Can dehydration really cause back muscle spasms?
Yes, dehydration can lead to an imbalance in electrolytes, which are essential for normal muscle function. This imbalance can cause muscles to contract uncontrollably, leading to spasms.
Are there specific exercises that can help reduce the risk of back muscle spasms?
Yes, exercises that strengthen the core and back muscles, improve flexibility, and promote good posture can help reduce the risk of back muscle spasms. Examples include yoga, Pilates, and specific back-strengthening exercises.
Can stress and anxiety directly cause back muscle spasms?
Yes, stress and anxiety can cause muscle tension and lead to spasms. The body’s stress response releases hormones that can increase muscle tightness and trigger spasms.
What role does nutrition play in preventing back muscle spasms?
Proper nutrition helps maintain a balance of electrolytes and essential minerals like potassium, calcium, and magnesium, which are crucial for muscle function. A balanced diet can help prevent muscle spasms.
Are there any long-term effects of untreated back muscle spasms?
Untreated back muscle spasms can lead to chronic pain, reduced mobility, and muscle weakness. They can also cause compensation in other muscles, potentially leading to additional problems.
Can poor posture cause back muscle spasms even if I’m not lifting heavy objects?
Yes, poor posture can strain the muscles and ligaments in the back, leading to spasms, even without lifting heavy objects. Maintaining good posture is important to prevent muscle strain.
Is it safe to exercise while experiencing a back muscle spasm?
It’s generally recommended to rest the affected muscles and avoid strenuous activities during a spasm. Gentle stretches and low-impact activities may be safe, but it’s best to consult a healthcare professional.
How can I differentiate between a muscle spasm and a more serious back injury?
Muscle spasms often involve sudden tightness and pain but usually improve with rest and home treatments. More serious injuries may involve severe pain, numbness, tingling, or weakness in the legs. If in doubt, seek medical evaluation.
Can sleeping positions affect the likelihood of back muscle spasms?
Yes, sleeping positions that do not support the natural curve of the spine can strain back muscles and lead to spasms. Using a supportive mattress and pillow can help maintain proper alignment.
Are there any specific medications that are particularly effective for back muscle spasms?
Over-the-counter pain relievers like ibuprofen or acetaminophen can be effective. Muscle relaxants may be prescribed for more severe spasms. Always consult a doctor before taking any medication.
How does physical therapy help with back muscle spasms?
Physical therapy helps by improving muscle strength, flexibility, and posture. Therapists can teach specific exercises and stretches that reduce spasms and prevent future occurrences.
Can certain activities or sports increase the risk of back muscle spasms?
Yes, activities and sports that involve repetitive movements, heavy lifting, or sudden twists and turns can increase the risk of back muscle spasms. Proper warm-up and technique are important.
Is it possible for back muscle spasms to cause referred pain in other parts of the body?
Yes, back muscle spasms can sometimes cause referred pain, meaning the pain is felt in another area of the body, such as the hips, legs, or shoulders.
Can massage therapy help with back muscle spasms?
Yes, massage therapy can help relax tight muscles, improve circulation, and reduce pain associated with back muscle spasms.
How does maintaining a healthy weight contribute to preventing back muscle spasms?
Maintaining a healthy weight reduces the strain on your back muscles and spine, lowering the risk of muscle spasms and other back problems.
Are there any specific stretching routines recommended for preventing back muscle spasms?
Yes, routines that include stretches for the hamstrings, hip flexors, and lower back can help prevent spasms. Examples include the child’s pose, knee-to-chest stretch, and the cat-cow stretch.
Can back muscle spasms occur without any physical activity?
Yes, back muscle spasms can occur without physical activity due to factors like poor posture, dehydration, or underlying medical conditions.
How does cold therapy help with back muscle spasms?
Cold therapy helps by numbing the sharp pain, reducing inflammation, and slowing down nerve impulses, which can reduce muscle contractions and spasms.
What is the role of heat therapy in treating back muscle spasms?
Heat therapy helps relax tight muscles, increase blood flow to the affected area, and promote healing by bringing more oxygen and nutrients to the muscles.
Can back muscle spasms be a symptom of fibromyalgia?
Yes, back muscle spasms can be a symptom of fibromyalgia, a condition characterized by widespread muscle pain and tenderness. If you suspect fibromyalgia, consult a healthcare professional for a proper diagnosis.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.