Ankylosing Spondylitis
Ankylosing spondylitis is a common issue for many individuals. Severe discomfort or pain that interferes with daily activities or is accompanied by swelling, redness, or warmth should be assessed by a healthcare provider.
At Complete Orthopedics, our specialized team is prepared to manage all types of ankylosing spondylitis, offering surgical treatments when necessary. We serve New York City and Long Island with six hospital locations, providing outstanding surgical and orthopedic care. You can schedule an appointment with our expert surgeons online or by phone.
Discover the common causes of ankylosing spondylitis and explore the treatment options we offer, including when surgery might be required.
Overview
Ankylosing arthritis (AS) is also known as Bechtrew disease is a type of inflammatory arthritis. Ankylosing spondylitis mostly involves the spine but may involve other peripheral joints as well. The management of ankylosing spondylitis has vastly improved with newer medication that halts the progression of the disease. Most patients benefit from medical therapy and only a few patients may require surgery for correction of the deformity.
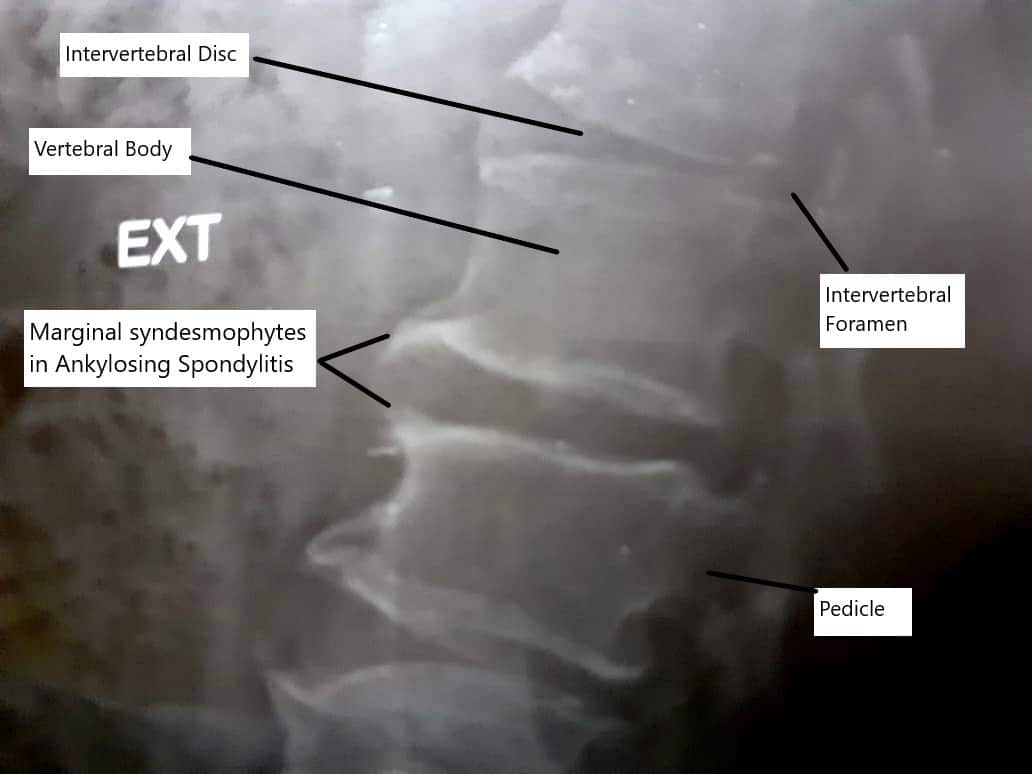
Syndesmophytes in Ankylosing Spondylitis
Affected Population
Younger patients in the age groups of 15-45 years are affected and males are more frequently affected than females. The disease may run in the family with a genetic marker of HLA B27, but not all HLA B27 patients have ankylosing spondylitis. Although, the majority of patients with ankylosing spondylitis have HLA B27 present.
Causes & Pathogenesis
The exact cause of ankylosing spondylitis is unknown but various genetic and autoimmune pathways play a role in its pathogenesis. The cells of the body that function to protect the body against foreign particles/cells such as infection start to malfunction. These immune cells recognize certain parts of the body as foreign and attack these structures. The primary target of these cells in ankylosing spondylitis is bone/cartilage interface, especially at the site of insertion of tendon/ligaments in the bone (enthesis).
The inflammation of the enthesis leads to the destruction and erosion of the bone and the surrounding soft tissues. The autoimmune destruction eventually leads to ossification of the soft tissue structures and bony fusion of the involved joint. In ankylosing spondylitis, the joint where the lower spine meets with the pelvic bone (sacroiliac joint) is most commonly involved.
The repair process that follows the destruction of the enthesis in ankylosing spondylitis leads to bone formation (ossification) in the soft tissues. There is inflammation of the outer ring of the intervertebral disc and subsequent fusion of the involved vertebrae through osteophytes (syndesmophytes).
Symptoms
There is typically a low back pain that improves with activity and gets worse with rest. The patients complain of morning stiffness in the back that lasts more than 30 minutes. Occasionally the patients may wake up at night secondary to pain.
There may be systemic manifestations of the ankylosing spondylitis in the form of inflammation of the eyes and amyloid deposition disease of the lungs or kidney, etc.
Besides the spine, other peripheral joints may be involved in ankylosing spondylitis. The large joints in the lower extremities such as hip joints may be more commonly involved than shoulder joints. Like the sacroiliac joint, other sites of enthesis may be involved such as the Achilles tendon in the ankle, plantar fascia in the feet, and pubic symphysis in the pelvis.
Spine Deformity
Spinal deformity is one of the leading causes of morbidity and mortality in ankylosing spondylitis. The patient may form a hunched back deformity of the spine (kyphotic deformity). In the initial stages, the patient tries to compensate for the hunched back deformity by bending their knees and extending their hips while standing/walking. In the advanced stages when the hips also get involved, the patient’s spine deformity becomes more apparent.
To compensate for the loss of the forward vision from the hunched back, the patient tries to extend the neck. As the disease progresses the ability to extend the neck is limited and leads to the characteristic ‘chin in the chest’ position. The patient then tries to compensate by rolling his/her eyes upward to look forward.
The kyphotic deformity continues until the rib cage bends forward to meet the bony pelvis in the front. This may compress the abdominal organs and interfere with their function. The patient is unable to inflate and deflate their lungs fully during breathing leading to difficulty breathing. The ankylosed (fused) spine becomes vulnerable to fractures with minimum trauma. Extension fractures may occur in the cervical spine followed by the thoracic spine.
Diagnosis
The diagnosis of ankylosing spondylitis is made by the orthopedic surgeon after extracting a thorough history and conducting a detailed physical examination. The surgeon may measure the chest expansion and the flexibility of the lower spine upon bending forward.
Blood investigations form an important part in the diagnosis of ankylosing spondylitis. The physician may subject the blood to look for markers of inflammation such as ESR, CRP, anti-CCP, and HLA B27 to look for genetic association. Radiological investigations in the form of X-rays are done in special views to look for erosion and ossification. The physician may also request a CT scan or an MRI for a more detailed evaluation. While CT scan is very sensitive to bony abnormalities, an MRI is the best modality for the detection of AS in young patients.
Classification
Modified New York criteria are used to diagnose ankylosing spondylitis. Ankylosing spondylitis is diagnosed if the radiological criteria is met with at least one clinical criteria. The radiological criteria consist of grade 2 or more sacroiliitis (inflammation of SI joint) on both the SI joints on plain X-ray or grade 3 or 4 sacroiliitis on one of the SI joints.
The clinical criteria consist of:
- Low back pain and stiffness persisting for more than 3 months which improves with exercise but not rest, or
- Limitation of movement in the lumbar spine in both front to back and side to side motion planes, or
- Limitation of chest expansion
Treatment
Medical therapy is the mainstream treatment after the initial diagnosis of ankylosing spondylitis. Nonsteroidal anti inflammatory medications are the first choice medications and are given continuously. The medications are carefully balanced in the view of gastritis and bleeding diathesis.
Disease modifying anti rheumatic drugs (DMARDS) such as sulfasalazine and methotrexate may be used when the NSAIDs fail to act. Corticosteroids and TNF alpha inhibitor medications may be used as well. The medications are given keeping in mind their interactions and side effects.
The surgical management in ankylosing spondylitis is reserved for patients in whom the disease causes strong limitation of daily life. The surgical management is also done for patients with neurological symptoms, progressive deformity, chronic pain, and fractures.
The type of surgery depends upon the indication for the surgery. Bone cutting surgery or osteotomies together with lumbar fusion surgery may be done to correct the deformity and restore the balance of the spine.
Living with Ankylosing Spondylitis
While there is no cure for AS, there are several treatments and lifestyle changes that can help manage the symptoms and improve quality of life.
Medications:
-
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These are usually the first line of treatment to reduce pain and inflammation.
- Biologic Medications: These are used for more severe cases. They target specific parts of the immune system to reduce inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): These can help slow the progression of AS.
- Pain Relievers: Over-the-counter or prescription pain medications can help manage pain.
Physical Therapy and Exercise:
-
- Physical Therapy: A physical therapist can design a program tailored to your needs to maintain flexibility and posture.
- Regular Exercise: Staying active is crucial. Activities like swimming, yoga, and stretching can help maintain mobility and reduce pain.
Healthy Lifestyle Choices:
-
- Posture: Paying attention to your posture and using supportive chairs can help reduce pain.
- Diet: Eating a balanced diet and maintaining a healthy weight can reduce stress on your joints.
- Quit Smoking: Smoking can worsen AS symptoms and increase the risk of complications.
Complications of Ankylosing Spondylitis
AS can lead to several complications if not managed properly:
- Eye Inflammation (Uveitis): This can cause pain, redness, and blurred vision. It’s essential to see an eye specialist if you experience these symptoms.
- Heart Problems: AS can increase the risk of heart disease and aortic valve problems.
- Lung Issues: Inflammation and fusion of the ribs can limit lung expansion, making breathing difficult.
- Spinal Fractures: The bones in the spine can become brittle and more prone to fractures.
Psychological Impact
Living with a chronic condition like AS can take a toll on mental health. It’s not uncommon to experience feelings of frustration, anxiety, or depression. Support from family, friends, and healthcare providers is crucial. Counseling or joining a support group can also be beneficial.
Do you have more questions?
What are the early signs of Ankylosing Spondylitis?
Early signs of Ankylosing Spondylitis include chronic back pain and stiffness, particularly in the lower back and hips, that is worse in the morning or after periods of inactivity. Other early symptoms can include fatigue and pain in the shoulders, neck, or other joints.
How does Ankylosing Spondylitis affect daily activities?
AS can make daily activities challenging due to pain, stiffness, and reduced flexibility. Tasks that involve bending, lifting, or twisting can become difficult. Maintaining good posture and using ergonomic tools can help manage these challenges.
Are there any specific exercises recommended for people with AS?
Yes, exercises that improve flexibility, strength, and posture are beneficial. Swimming, yoga, and stretching exercises are particularly recommended. It’s important to work with a physical therapist to develop a personalized exercise plan.
Can diet influence the symptoms of AS?
While no specific diet has been proven to cure AS, maintaining a healthy, balanced diet can help manage symptoms. Foods rich in omega-3 fatty acids, such as fish, and anti-inflammatory foods like fruits and vegetables, can be beneficial.
How does AS affect sleep, and what can be done to improve it?
AS can affect sleep due to pain and discomfort. Using a firm mattress, maintaining good sleep hygiene, and managing pain with medications or hot/cold therapy before bedtime can improve sleep quality.
What are the long-term effects of Ankylosing Spondylitis?
Long-term effects can include chronic pain, spinal fusion, reduced mobility, and a stooped posture. Complications such as uveitis, heart disease, and lung problems can also occur if the condition is not managed properly.
Can Ankylosing Spondylitis be misdiagnosed?
Yes, AS can be misdiagnosed, especially in its early stages, because its symptoms overlap with other types of back pain and arthritis. A thorough medical evaluation, including imaging and genetic tests, is essential for an accurate diagnosis.
Is there a genetic test for Ankylosing Spondylitis?
Yes, testing for the HLA-B27 gene can support the diagnosis of AS. However, having the HLA-B27 gene does not necessarily mean you will develop AS, and not all individuals with AS carry this gene.
What is the role of biologic medications in treating AS?
Biologic medications target specific components of the immune system to reduce inflammation. They are typically used when other treatments, like NSAIDs, are not effective. Examples include TNF inhibitors and IL-17 inhibitors
Can women get Ankylosing Spondylitis, and are their symptoms different from men’s?
Yes, women can get AS. While it is more common in men, women can experience similar symptoms, though they may have more peripheral joint involvement (like the knees and wrists) and less spinal fusion compared to men.
How often should someone with AS see their doctor?
Regular follow-ups with a rheumatologist or orthopedic specialist are important. The frequency of visits can vary based on the severity of symptoms and treatment plan, but typically, every 3-6 months is recommended.
Are there any surgical options for AS, and when are they considered?
Surgery is considered when there is severe joint damage, spinal deformities, or when conservative treatments fail to relieve symptoms. Procedures may include joint replacement or spinal surgery to correct severe deformities.
What lifestyle changes can help manage AS symptoms?
Regular exercise, maintaining good posture, quitting smoking, and managing stress can help manage AS symptoms. Additionally, following a healthy diet and maintaining a healthy weight are beneficial.
Can pregnancy affect Ankylosing Spondylitis?
Pregnancy can affect AS symptoms, with some women experiencing a decrease in symptoms while others may see an increase. It is important to work closely with healthcare providers to manage AS during pregnancy.
Is Ankylosing Spondylitis considered a disability?
AS can be considered a disability, particularly if it significantly impacts daily activities and work. Eligibility for disability benefits varies by country and specific criteria.
What advancements are being made in the treatment of AS?
Research is ongoing to better understand the genetic and environmental factors of AS. Advances in biologic medications and the development of new therapies targeting specific immune pathways are promising.
Can alternative therapies help with AS symptoms?
Some people find relief from alternative therapies such as acupuncture, massage, and chiropractic care. However, these should complement, not replace, conventional medical treatments.
How does AS affect mental health, and what can be done about it?
Chronic pain and disability from AS can lead to depression and anxiety. Mental health support through counseling, support groups, and medication can be important aspects of comprehensive care.
What is the prognosis for someone with AS?
The prognosis varies. With early diagnosis and proper management, many people with AS can lead productive lives. However, without treatment, AS can lead to severe complications and reduced quality of life
Can children develop Ankylosing Spondylitis?
Yes, AS can begin in childhood, a condition known as juvenile ankylosing spondylitis. Symptoms in children can include pain and stiffness in the spine and peripheral joints.
How does Ankylosing Spondylitis affect work life?
AS can affect work life by limiting mobility and causing chronic pain. Adjustments such as ergonomic workstations, flexible hours, and regular breaks can help manage symptoms.
Can physical therapy alone manage AS symptoms?
Physical therapy is a crucial part of managing AS, but it is usually combined with medications and other treatments for optimal management of symptoms.
What are the warning signs that AS is getting worse?
Worsening AS symptoms include increased pain and stiffness, reduced range of motion, new joint pain, eye redness or pain, and symptoms of heart or lung involvement. It’s important to report these to your doctor promptly.
Are there specific sleep positions that can help with AS pain?
Sleeping on your back with a firm mattress and avoiding pillows under your neck or knees can help maintain a neutral spine position. Some people also find relief by sleeping on their sides with a pillow between their knees.
How does stress impact Ankylosing Spondylitis?
Stress can exacerbate AS symptoms by increasing inflammation and pain sensitivity. Stress management techniques such as mindfulness, relaxation exercises, and physical activity can help reduce the impact of stress on AS.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
