Case Study: Management of Lumbar Canal
Stenosis in a 63-year-old Female
The patient is a 63-year-old female who presented with complaints of worsening radiating pain along the back of both thighs more on the left side than right for many weeks. The patient reports she has had radiating back pain since the past four that started after a slip and fall. The patient worked in a warehouse and her job involved repetitive lifting and pushing. She is currently not working.
The patient describes the pain as a sharp shooting sensation in the back of the thighs. The pain is associated with numbness and tingling in both the lower extremities. For the past six months, the patient reports a worsening numbness in both legs (left more than right). The patient also reports weakness in the left leg and a feeling of clumsiness in the left foot.
The patient previously had tried and exhausted various conservative measures for lower back pain. She had epidural and nerve root injection last year but the relief did not last long. Physical therapy was also tried extensively but without much relief. She is a former smoker with a history of 20 pack years. She does not report any known drug allergies.
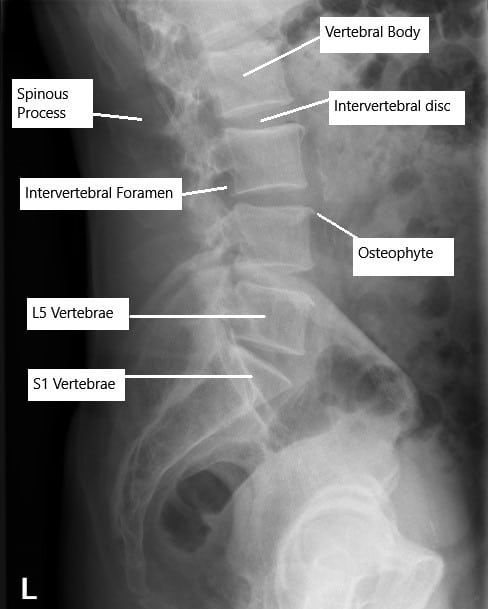
X-ray of the lumbar spine showing degenerative changes.
The patient’s past medical history is significant for diabetes mellitus and hypothyroidism, both well controlled with medication. The patient denies any recent onset of fever, chills, or rigors. The patient denied any recent onset of bowel or bladder dysfunction.
On physical examination, there is a paravertebral muscle spasm bilaterally around the L4-L5 region. There is a limited range of motion of the spine due to discomfort. The straight leg raise test is positive at 55 degrees. There is no tenderness to palpation over the trochanteric bursa and hip. The patient walks with an antalgic gait and uses a cane for ambulation.
The power sensory examination of both lower extremities revealed a decreased DTR ⅗ in the left ankle and knee. There was a sensory loss over the side of the left foot and first web space. There is no soft tissue swelling and ecchymosis. The patient has a full range of motion of the hips. The hips are stable on the examination.
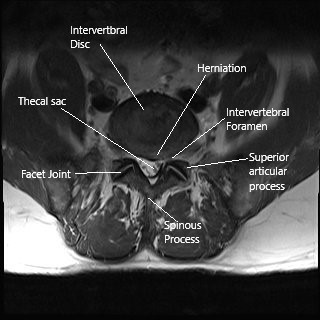
MRI axial section of the lumbar spine showing foraminal stenosis.
MRI of the lower spine revealed an L4-L5 diffuse disc bulge with superimposed right central
subarticular and foraminal disc protrusion (disc herniation) and intermediate-grade central canal and high-grade foraminal stenosis, right greater than left. There is an L5-S1 shallow left central and subarticular disc protrusion (disc herniation).
Various treatment options were discussed and the patient opted for surgical management. We discussed the risks, benefits, and complications of either treatment and the patient signed informed consent.
PREOPERATIVE DIAGNOSES:
- Stenosis, central and lateral L4-5 bilaterally.
- Disc herniation, lateral recess, and foraminal stenosis of left side L5-S1.
POSTOPERATIVE DIAGNOSES:
- Stenosis, central and lateral L4-5 bilaterally.
- Disc herniation, lateral recess, and foraminal stenosis of left side L5-S1.
OPERATION:
- Laminotomy, L4 on the right.
- Laminotomy, L4 on the left.
- Laminotomy, L5 on the left.
- Neurolysis and decompression of L5 bilaterally.
- Neurolysis, decompression, foraminotomy of the left S1 nerve root.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where general anesthesia was induced. The patient was intubated. The patient was turned prone onto the Jackson table with Wilson’s frame. All the bony prominences were well padded. The preop antibiotic was given. Time-out was called. The lower back was prepped aseptically and draped in the usual fashion. The area was localized using a spinal needle and a lateral x-ray.
An incision was given from the inferior L4 to superior S1. With the use of Bovie, dissection was performed along either side of the spinous process of inferior L4 as well as on the left side of L5. The lamina was exposed on both sides at L4 and the left side at L5.
The level was again checked on the C-arm. Laminotomy of bilateral L4 was performed using high-speed matchstick burr. The laminotomy of L5 on the left side was also performed similarly. The midline structures were left intact to save from the tension band. After the laminotomy, the ligamentum flavum was excised first from the left side of L4, then from the right side of L4, and then left L5.
The decompression of lateral, foraminal decompression of left L4, left L5, and right L4 was
performed using Kerrison punches 2, 3, 4 mm. Neurolysis of Bilateral L5 and left S1 was performed with Woodson and Penfield 4 and nerve hook. Decompression was checked with the use of the Woodson tool. Hemostasis was thoroughly achieved.
The disc was checked anteriorly especially at L5 and was found to be calcified. No attempt was done to remove the disc. The decompression was found to be satisfactory. The wound was thoroughly washed. Hemostasis was achieved. A picture was taken with Woodson dental tool in left L5 and Penfield #4 on the right L4 foramina to confirm our decompression.
Surgifoam mixed with 40 mg of Depo-Medrol was instilled. The closure was done in layers using #0 Vicryl, #2-0 Vicryl, and #4-0 Monocryl. Vancomycin 1 g was also instilled into the wound. The dressing was performed. The patient was turned supine and extubated and moved to recovery in a stable condition.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
