Case Study: Minimal Invasive (Tubular) Right L5 Laminotomy
with L5-S1 Microdiscectomy and S1 Nerve root neurolysis
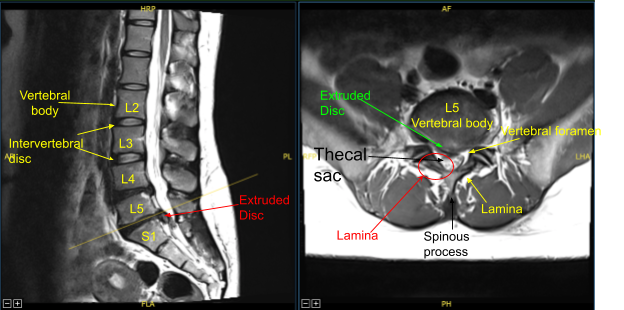
The patient presented with signs and symptoms of right lower extremity weakness with a very large herniated intervertebral disc at L5-S1 on the MRI causing severe compression of the thecal sac and S1 nerve root on the right side. Due to neurological deficit and severe pain, surgery was recommended to decompress the lumbar spine.
The risks, benefits, alternatives and potential complications were explained. All questions were answered until no further issues were raised and The patient provided written informed consent which was placed in the chart.
The patient was brought to the operating room. Timeout was performed. General anesthesia was induced. The patient was intubated by the Anesthesia Service.
Respiratory and cardiac monitoring leads were placed. Neuromonitoring leads for somatosensory evoked potentials and EMG were placed and baseline signals were obtained.
The patient received preoperative prophylactic IV antibiotics. The patient was positioned prone on a Wilson frame. All pressure points were carefully padded. Lumbar area was cleaned with chlorhexidine and sterilized with DuraPrep solution.
Sterile drapes were placed in the usual manner. The C-arm unit was draped sterilely. Operative microscope was balanced and draped sterilely, and the surgery was performed using microsurgical instruments and techniques for visualization performing micro dissection for decompression.
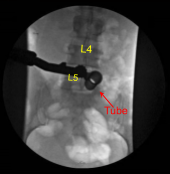
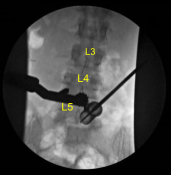
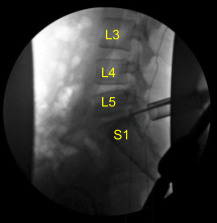
A 22-gauge spinal needle was used to localize the L5-S1 level. A marking pen was used to demarcate the midline. An 18 mm vertical incision adjacent to the spinous process on the right side was demarcated. 1% lidocaine with epinephrine was infused.
The skin was opened with a #15 blade scalpel. Hemostasis was obtained with Bovie. Bovie was used to sharply divide the fascia. Sequential dilators were used to dock a 16 mm diameter x 4 cm tubular retractor which was affixed rigidly to the bed frame.
Operative microscope was brought into the field for micro dissection using micro surgical instruments and techniques for the remainder of the procedure. Bovie, monopolar and pituitary rongeurs were used to resect the overlying
soft tissue over the right L5 lamina.
An electric high-speed drill with sterile irrigation was used to perform right L5 laminotomy exposing the ligamentum flavum which was detached rostrally from the ventral lamina with an angled curette and reflected caudally and then resected in a piecemeal fashion with 2 and 3 mm Kerrison rongeurs exposing the intact dura.
The Right S1 nerve root appeared splayed under pressure and inflamed. There was a herniated disc apparent in the axilla between the thecal sac and the right S1 nerve root.
Penfield micro dissector was used to explore the ventral epidural space and then a nerve root retractor was used to retract the S1 nerve root. Various nerve hooks were used to resect the disc herniation which was removed with micro pituitary rongeurs.
The herniated disc fragments were collected and sent to pathology for analysis. An annular defect was identified and extended with a bayoneted #15 blade scalpel.Neurolysis was performed with micro instruments of the S1 nerve root enabling sufficient retraction to fully remove the multiple herniated disc fragments until circumferentially the S1 nerve root was completely decompressed as well as the ventral thecal sac. This was confirmed with nerve hooks, Penfield micro instruments and fluoroscopy.
Hemostasis was confirmed with bipolar electrocautery and Surgiflo hemostatic matrix. The wound was irrigated clear. 40 mg of Depo-Medrol steroid was left in the epidural space. The tubular retractor was removed. Again, bipolar was used to perform hemostasis at the muscle while withdrawing the tubular retractor.
The microscope was then brought out of the field. The wound was closed in layers including 2-0 Vicryl sutures for the fascia. Exparel long acting local anesthetic was then infused into soft tissues.
The subdermal layer was closed with 2-0 Vicryl sutures and the skin was reapproximated with a running subcuticular 4-0 Monocryl which was cleaned, dried sterilely and dressed with Prineo Dermabond dressing followed by Telfa and Tegaderm.
The patient was turned supine on the cart, extubated uneventfully and transported to the recovery room in stable condition. At the end of the case, all sponge counts, needle counts, and instruments counts were correct. The patient tolerated the procedure well.
Patient followed up one week after surgery and stated they had observed improvements with. The patient continued to follow up as an outpatient for 4,6 and 8 weeks after the surgery
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.

