Ossification of Posterior Longitudinal Ligament
Ossification of posterior longitudinal ligament (OPLL) is a condition affecting the cervical spine. OPLL may lead to compression of the spinal cord and may cause symptoms of cervical myelopathy. Patients with cervical myelopathy present with symptoms of weakness and clumsiness in the hands and difficulty walking.
Anatomy of Cervical Spine
The ligaments in the spine function to provide structural support to the vertebral column. The ligaments also keep a check to prevent excessive motion in the range of movement. The spinal cord lies inside the central vertebral canal formed in the front but the vertebral body and the lamina at the back.
The posterior longitudinal ligament is present in the vertebral body’s back (front of the spinal cord). The ligament flavus is present in the back of the spinal cord.
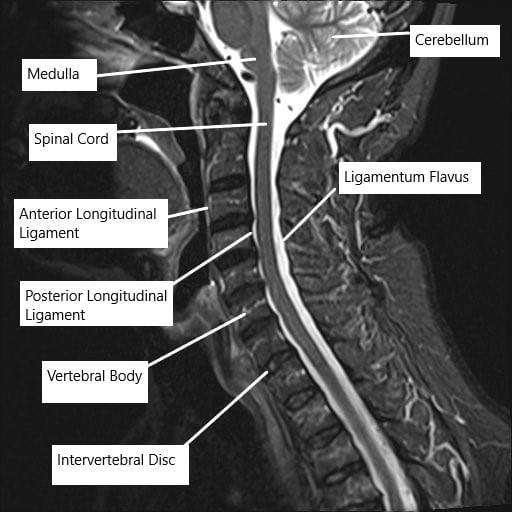
MRI of the cervical spine showing the various ligaments surrounding the spinal cord.
Ossification of Posterior Longitudinal Ligament Causes & Pathology
Ossification means the formation of bone tissue in any tissue. The posterior longitudinal ligament is a flexible ligament which is naturally not ossified. The ossification in OPLL causes the ligament to become rigid and grow in size. The increased size may decrease the precarious space in the vertebral canal already occupied by the spinal cord and its coverings.
The enlargement of the ligament occurs most commonly in the cervical spine and may compress the spinal cord. The compression of the spinal cord may cause symptoms of cervical myelopathy. The ossification of posterior longitudinal ligament occurs most frequently in patients of Asian ancestry, particularly Japanese.
The exact cause of ossification of posterior longitudinal ligament has been unclear but has been thought to be caused by various factors. Diabetes, mechanical factors, a diet rich in salt, high body weight, and genetics have been associated with the ossification of the posterior longitudinal ligament.
Ossification of Posterior Longitudinal Ligament Symptoms
The symptoms of OPLL may be mild at first as the disease has a slow progression but may be accelerated in some cases. The patients may complain of pain and stiffness in the neck. There may be symptoms of altered sensation in the arms and hands. Patients may complain of feeling numbness and tingling in the upper extremities.
As the disease progresses and the compression of the cord increases, the patients may complain of clumsiness in their hands. They may experience difficulty in holding and manipulating objects. There may be difficulty walking and navigating stairs. The patients may complain of weakness in the lower extremities. In rare cases, there may be loss of bowel and bladder control.
Diagnosis
The physician extracts a thorough history and establishes a timeline of the symptoms. The physician conducts a thorough physical examination. The physical examination includes tests to look for the patient’s walking pattern, the strength in the arms and the legs, and the sensation in all four limbs.
The radiological examination includes an X-ray, CT scan and an MRI. The X-ray is usually the first imaging done in suspected OPLL. The physician is able to see the bone structure as well as ossification of the posterior longitudinal ligament.
A CT scan provides a more detailed image of the bone structures as compared to an X-ray. The MRI scan is able to discern the soft tissue structures including the spinal cord. MRI myelography may be done in patients who are unable to have a regular MRI.
Management
Nonoperative management is done in patients with mild disease. The patients are regularly followed up for observation. The conservative modalities include medications such as nonsteroidal anti-inflammatory medications and physical therapy to improve strength and flexibility.
Surgical management forms the mainstream treatment for patients with functional degradation. The surgical management is done in the form of decompression and stabilization. Different approaches may be used depending upon the patient’s anatomy and the disease process.
The decompression part of the surgery involves removing all the bony/soft tissue structures compressing the spinal cord. The segment of spine is then fused together to eliminate any motion in between the involved vertebrae. The elimination of motion provides stability and prevents any further compression.
The surgeon may access to decompress and fuse the spine either from the front, known as anterior cervical decompression and fusion. Or the surgeon may approach from behind the neck, known as posterior cervical decompression and fusion. In some cases, both anterior and posterior approaches may be used to relieve compression.
Majority of the patients experience significant relief from their symptoms after the surgery. There may be some loss of movement in the range of motion of the neck owing to the fusion.
Do you have more questions?
What causes OPLL?
The exact cause is unknown, but it is believed to be due to a combination of genetic, hormonal, and environmental factors. There are associations with conditions like diabetes and obesity, and it is more common in East Asian populations
How is OPLL diagnosed?
Diagnosis typically involves a combination of patient history, physical examination, and imaging studies like X-rays, MRI, and CT scans to identify the ossification and assess the extent of spinal cord compression
What are the symptoms of OPLL?
Symptoms include neck pain and stiffness, radiating pain to the shoulders and arms, numbness or tingling in the hands, weakness in the arms and legs, difficulty with coordination and balance, and in severe cases, paralysis or bladder and bowel dysfunction
What non-surgical treatments are available for OPLL?
Non-surgical treatments include pain relievers, anti-inflammatory drugs, muscle relaxants, physical therapy, and lifestyle modifications such as weight management and avoiding activities that exacerbate symptoms
What surgical options are available for treating OPLL?
Surgical options include anterior approaches like ACDF and corpectomy, posterior approaches like laminoplasty and laminectomy, and sometimes combined approaches for more extensive cases
When is surgery recommended for OPLL?
Surgery is recommended when conservative treatments fail to relieve symptoms or if there is significant spinal cord compression that poses a risk of severe neurological damage
What is the recovery process like after OPLL surgery?
Recovery involves rest, medication, and physical therapy. Patients are typically advised to follow a tailored physical therapy program, avoid strain on the neck and spine, and monitor for complications
How successful is OPLL surgery?
Surgical outcomes are generally favorable, with many patients experiencing significant relief from symptoms and improved quality of life. However, some may continue to have residual symptoms or complications
What are the risks associated with OPLL surgery?
Risks include infection, bleeding, spinal fluid leakage, nerve damage, and worsening of neurological symptoms due to spinal cord manipulation
Can OPLL recur after surgery?
While surgery can relieve symptoms and stabilize the spine, there is a risk of recurrence. Ongoing follow-up and possibly further treatment may be necessary
What role does genetics play in OPLL?
Genetics is believed to play a significant role in OPLL, with certain genetic markers associated with an increased risk. This is particularly evident in populations with a higher prevalence of the condition
Are there any lifestyle changes that can help manage OPLL?
Yes, weight management, proper posture, regular exercise, and avoiding activities that strain the neck and spine can help manage OPLL symptoms
How does OPLL progress over time?
OPLL can progress slowly, with gradual worsening of symptoms as the ossification increases and further compresses the spinal cord and nerves. Early intervention can help manage the progression
Can physical therapy help with OPLL?
Yes, physical therapy can help strengthen the neck muscles, improve flexibility, and reduce pain. A tailored physical therapy program is an important part of both conservative treatment and postoperative recovery
Is there a cure for OPLL?
There is no cure for OPLL, but treatments can effectively manage symptoms and prevent further progression. Research into the genetic and molecular mechanisms of OPLL may lead to new therapeutic approaches in the future
What is the difference between laminoplasty and laminectomy?
Laminoplasty involves reshaping or repositioning the lamina to relieve pressure on the spinal cord while maintaining stability. Laminectomy involves removing the lamina to create more space for the spinal cord, often combined with spinal fusion for stability
How long does it take to recover from OPLL surgery?
Recovery time varies depending on the type of surgery and the patient’s overall health, but it typically takes several weeks to months. Full recovery and return to normal activities can take up to a year
What are the potential complications of not treating OPLL?
Untreated OPLL can lead to severe spinal cord compression, resulting in chronic pain, significant neurological deficits, and in extreme cases, paralysis and loss of bladder and bowel control
Can children develop OPLL?
OPLL is rare in children and is more commonly seen in middle-aged and older adults. However, it can occur in younger individuals, particularly those with a genetic predisposition
How does OPLL differ from other spinal conditions like spondylosis or disc herniation?
OPLL involves the ossification of a specific spinal ligament, whereas spondylosis refers to general degenerative changes in the spine, and disc herniation involves the displacement of the intervertebral disc material. Each condition has distinct causes, symptoms, and treatment approaches
Are there any new treatments or research developments for OPLL?
Research is ongoing to better understand the genetic and molecular mechanisms of OPLL, which may lead to new treatments. Advances in imaging and surgical techniques are also improving the diagnosis and management of the condition
What should I do if I suspect I have OPLL?
If you have symptoms suggestive of OPLL, such as neck pain, numbness, or weakness, you should seek medical evaluation. An orthopedic surgeon or spine specialist can perform the necessary diagnostic tests and recommend appropriate treatment
Can OPLL affect other parts of the spine besides the cervical region?
Yes, while OPLL is most commonly found in the cervical spine, it can also occur in the thoracic and lumbar regions, though less frequently
How does the surgical approach for OPLL get decided?
The choice of surgical approach depends on the extent and location of ossification, the patient’s overall health, and the surgeon’s experience. Detailed imaging studies and thorough patient evaluation guide the decision-making process

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
