Prolapsed Intervertebral Disk (PIVD)
If spine pain becomes severe enough to interfere with your daily routine or is associated with swelling, tenderness, or redness, it’s important to seek medical attention.
At Complete Orthopedics, our team of expert spine specialists is adept at managing spine pain with both surgical and non-surgical techniques. We examine your symptoms, determine the underlying issue, and recommend the best treatment options, including surgery if required.
Serving New York City and Long Island, we are affiliated with six hospitals, offering cutting-edge spine surgery and comprehensive orthopedic services. You can schedule a consultation with our orthopedic surgeons either online or by phone.
Learn about the common causes of spine pain and explore the various treatment options available, including when surgery might be necessary.
Overview
PIVD, or Prolapsed Intervertebral Disc, is a condition that occurs when the material inside a spinal disc bulges or ruptures through the outer layer and compresses the nerves in the spinal canal. This can cause pain, numbness, weakness, and other symptoms.
PIVD can be caused by age-related wear and tear, injury, or degenerative conditions. Treatment options range from conservative measures like rest and physical therapy to more invasive procedures like surgery. If you suspect you may have PIVD, it’s important to seek medical attention to determine the best course of action for your specific case.
The herniated disk also known as the prolapsed intervertebral disk is a condition affecting the spine frequently causing neck pain or back pain. The intervertebral disk is a disc-shaped circular tissue present between the adjacent vertebrae. The disk acts as a cushion between two vertebrae and provides stability.
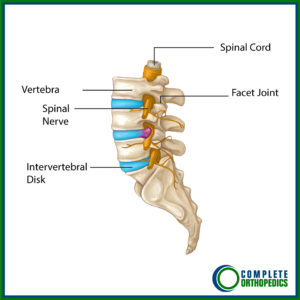
Anatomy of the Intervertebral disk
The intervertebral disks consist of a thick fibrous outer layer known as the annulus and a soft center known as the nucleus pulposus. The outer layer adjoining the vertebrae is known as the endplate. The endplate is formed by cartilage that contributes to the growth of the vertebra. The endplate is thick in childhood and gradually decreases in thickness.
The annulus fibrosis consists of concentric layers of thick fibers which imparts it the property of elasticity while being tough. The nucleus pulposus has a watery gel-like consistency giving it the ability to resist compression and allow cushioning action. The sinuvertebral nerve arises from the dorsal root ganglion and supplies the most superficial layer of the annulus fibrosis.
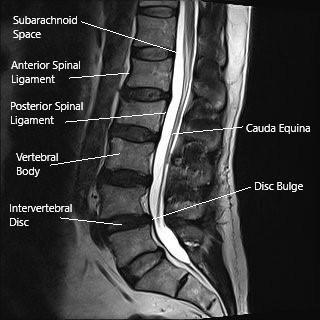
MRI of the lumbar spine in the sagittal section showing disc bulge.
A disc herniation results from the protrusion/extrusion of the nucleus pulposus through the annulus fibrosis of the disk. The vertebral canal has only enough room for the spinal cord/spinal nerves and the spinal fluid. The herniated disk causes inflammation and impinges/compresses the nerves/spinal cord causing symptoms of pain.
Classification based on anatomy
The herniated disc may either occur in the form of protrusion where the nucleus pulposus is still covered by a thin layer of the annulus fibrosis. In the case of disk extrusion, the nucleus pulposus herniates through the annulus fibrosis but is still contained within the disc space. In cases where the herniated nucleus pulposus loses contact with the original disk material, it is known as disk sequestration.
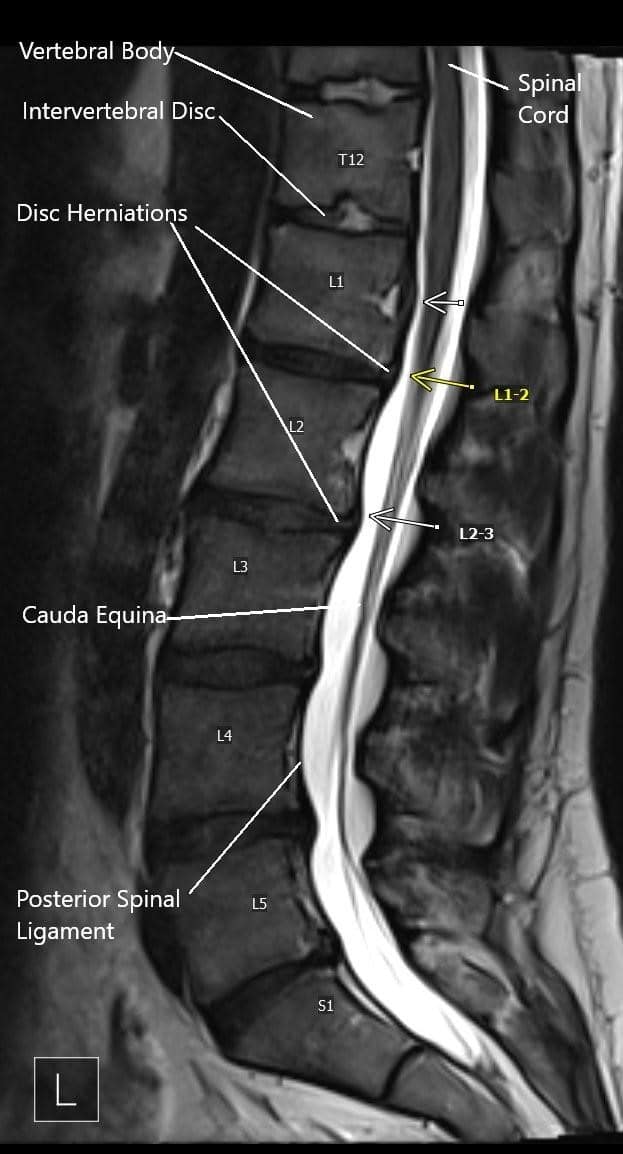
MRI image showing multiple disc herniations.
Classification based on location
The disk may herniate centrally known as central disk herniation. The disk material commonly compresses the spinal cord and in severe cases may result in cauda equina syndrome. Most frequently, the disk material herniated to the sides known as posterolateral/paracentral disk herniation.
In paracentral disk herniation descending nerve roots are commonly compressed leading to symptoms of pain in the area supplied by the nerve. Less commonly, the disk may herniate at extreme sides known as foraminal (far lateral) herniation. In foraminal herniation, the nerve exiting the foramen is impinged leading to symptoms.
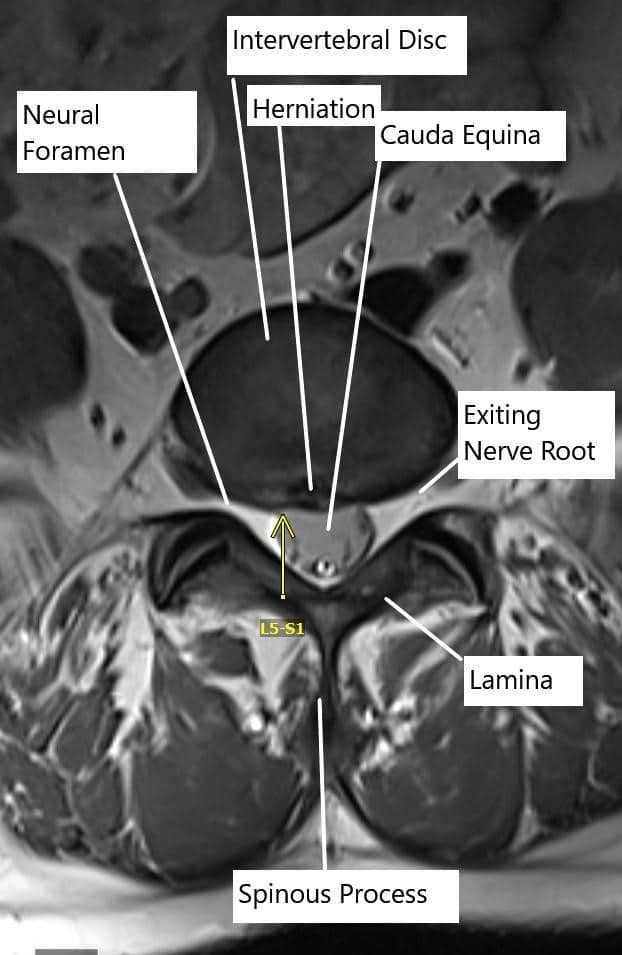
Axial section of the spine showing central disc herniation.
Prolapsed Intervertebral Disk Causes
The herniated disk in the majority of the cases occur in the lower back (lumbar spine) and the rest of the cases involve the neck (cervical spine). The prolapsed intervertebral disk is more common in adults aged 30 and more as with age the nucleus pulposus starts losing the water content, making it more susceptible to injuries.
Repetitive activities such as bending, turning, twisting may cause tears in the annulus. Obesity, smoking, and improper posture while sitting or standing to make the disks more vulnerable to injuries resulting in PIVD. Lifting weights and traumatic injuries frequently result in PIVD.
Prolapsed Intervertebral Disk Symptoms
The symptoms of a herniated disk depend on the location of the herniation and the amount of compression on the neural structures. In the lower back, a herniated disk commonly results in pain of the lower back. The patients may also experience shooting pains in the buttocks radiating to the back of the legs and feet. Some patients may complain of numbness and tingling of the feet or legs. Patients may also experience weakness of the legs or feet.
Cauda equina syndrome results from compression of the nerve roots from a large central disk herniation below the L1-L2 vertebrae. The compression of the sac below this level may result in loss of bowel bladder control, numbness of the saddle area. The condition is an emergency and requires immediate surgery.
The symptoms from disk herniation in the neck may result in pain in the region between the neck and the shoulders. The patients may experience radiating pain down the shoulders, arm, forearm, and hand. There may be numbness and tingling in the region supplied by the impinged nerve. The patients may complain of weakness of the muscles of the hand, forearm, arm, or shoulders depending upon the location of the impingement.
Prolapsed Intervertebral Disk Diagnosis
The diagnosis of a herniated disk is made by your examining physician. An extensive history is obtained regarding the onset of the symptoms and the activities leading to the symptoms. The physician will usually perform an extensive physical examination. The physical examination consists of different tests used to illicit the symptoms to localize the area of herniation. The physician will also assess the motor and sensory functions of the limbs.
Prolapsed Intervertebral Disk Management
The vast majority of the cases of prolapsed intervertebral disks respond to conservative/non-surgical treatment. The conservative management consists of rest and avoidance of activities precipitating the pain.
Nonsteroidal anti-inflammatory medication and muscle relaxants provide significant relief in the majority of the patients. Cold therapy provides symptom relief and heat therapy helps once the spasm has decreased.
The herniated disc material is slowly reabsorbed by the body which results in relief of the nerve impingement. Therefore most patients experience significant relief over a period of months. Once the pain subsides, the patients are advised to physical therapy to strengthen the muscles around the spine for providing better stability.
In cases, patients are unable to participate in physical therapy due to pain, epidural or foraminal steroid injection is given to provide relief from symptoms.
Rarely patients whose symptoms are not relieved with conservative therapy may require surgical intervention. Surgical management of lumbar disk herniations commonly consists of Microdiskectomy which is usually performed on an outpatient basis.
The surgery involves the use of a microscope to aid in performing the surgery through a very small incision in the back. The surgery involves the removal of the herniated disk and any part impinging upon the nerve root.
In the case of cervical disk herniation, surgical management usually consist of a fusion of the two adjoining vertebrae in addition to the removal of the disc material.

Shavers used for removing intervertebral disc material

Instruments used for lumbar spinal fusion
The instruments in the image above are used to remove the intervertebral disc material, create raw surface for the insertion of the bone cage and insert the pedicle screws.
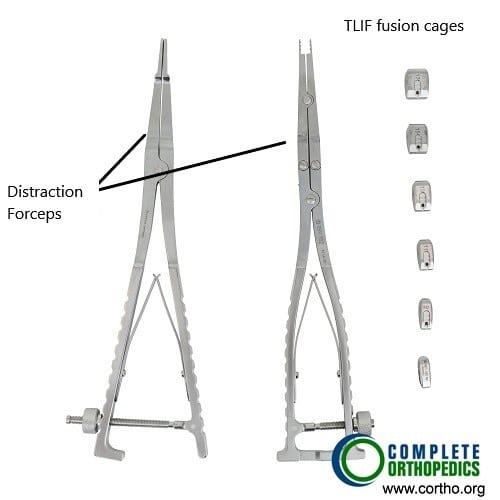
Distraction forceps and TLIF cages
The transforaminal lumbar interbody fusion (TLIF) utilizes a lateral incision from the back for fusion of the vertebrae. The image above shows distraction forceps used to create a space between the vertebra for insertion of the bone cage along with the bone graft material for aiding the fusion of the involved segment.
Do you have more questions?
What is PIVD?
PIVD is a condition where the inner gel-like material of a spinal disc bulges or ruptures through its outer layer, compressing the spinal nerves and causing pain and other symptoms.
What are the common symptoms of PIVD?
Symptoms include lower back pain, radiating pain to the legs, numbness, tingling, and weakness in the legs. For cervical PIVD, symptoms include neck pain, shoulder pain, radiating pain to the arms, and weakness in the arms.
What causes PIVD?
PIVD can be caused by age-related degeneration, repetitive activities, improper posture, obesity, smoking, lifting heavy weights, or traumatic injuries.
How is PIVD diagnosed?
Diagnosis involves a detailed medical history, physical examination, and imaging tests such as MRI or CT scans to identify the location and severity of the herniation.
What is disc sequestration?
Disc sequestration occurs when the herniated nucleus pulposus loses contact with the original disc material and is free in the spinal canal.
What is the difference between a protrusion and extrusion in PIVD?
Protrusion means the nucleus pulposus bulges out but is still covered by a thin layer of annulus fibrosis. Extrusion means the nucleus pulposus breaks through the annulus but remains connected to the disc.
Can PIVD heal on its own?
Yes, many cases of PIVD can improve over time with conservative treatment as the herniated material may be reabsorbed by the body.
What conservative treatments are available for PIVD?
Conservative treatments include rest, physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and heat/cold therapy.
When is surgery needed for PIVD?
Surgery is considered if conservative treatments fail to relieve symptoms, if there is significant nerve compression causing severe pain or weakness, or in emergencies like cauda equina syndrome.
What is Microdiskectomy?
Microdiskectomy is a minimally invasive surgery to remove herniated disc material and relieve nerve compression. It involves a small incision and the use of a microscope
What are the risks of PIVD surgery?
Risks include infection, bleeding, nerve damage, spinal fluid leak, and incomplete relief of symptoms.
What is spinal fusion surgery?
Spinal fusion involves removing the herniated disc and fusing two adjacent vertebrae with bone grafts and hardware to stabilize the spine.
How long is the recovery after PIVD surgery?
Recovery varies but typically involves several weeks of limited activity followed by physical therapy. Full recovery can take several months.
What lifestyle changes can help prevent PIVD?
Maintaining a healthy weight, practicing good posture, avoiding smoking, and performing regular exercises to strengthen the back and abdominal muscles can help prevent PIVD.
Can PIVD recur after treatment?
Yes, there is a risk of recurrence, especially if underlying factors like poor posture or repetitive strain are not addressed.
What exercises are recommended for PIVD?
Low-impact activities like walking, swimming, and specific stretching and strengthening exercises for the core muscles are recommended.
Can physical therapy help with PIVD?
Yes, physical therapy can help alleviate symptoms, improve mobility, and strengthen the muscles supporting the spine.
Are there any alternative treatments for PIVD?
Some patients find relief with chiropractic care, acupuncture, or massage therapy, but these should be considered complementary to conventional treatments.
How can I manage pain from PIVD at home?
Pain can be managed with over-the-counter pain relievers, alternating heat and cold therapy, and avoiding activities that exacerbate the pain.
Is it safe to exercise with PIVD?
Yes, but exercises should be low-impact and approved by your healthcare provider to avoid aggravating the condition.
What is cauda equina syndrome?
Cauda equina syndrome is a medical emergency caused by severe compression of the nerve roots below the L1-L2 level, leading to loss of bowel/bladder control and numbness in the saddle area.
What should I do if I suspect cauda equina syndrome?
Seek immediate medical attention as it requires urgent surgical intervention to prevent permanent damage.
Can PIVD cause permanent nerve damage?
If left untreated or if severe, PIVD can cause permanent nerve damage resulting in chronic pain, numbness, or weakness.
How does smoking affect PIVD?
Smoking decreases blood supply to the discs, accelerating degeneration and increasing the risk of PIVD.
Can weight loss help with PIVD symptoms?
Yes, losing excess weight can reduce the strain on the spine and alleviate PIVD symptoms.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
