Case Study: L4-S1 Posterior Instrumented Fusion
with L5-S1 Transforaminal Lumbar Interbody fusion
with Osteotomy
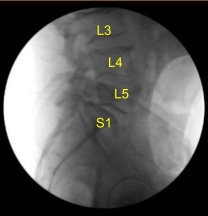
The patient presented to outpatient clinic status post motor vehicle accident with signs and symptoms of lumbosacral spondylolisthesis, bilateral L5 spondylolysis, L5 compression fracture, severe compression of L5 nerve root, and clinically with foot drop, severe radiculopathy and back pain. Surgery was recommended to decompress and stabilize the lumbosacral spine.
The risks, benefits, alternatives and potential complications were explained to him. All questions were answered until no further issues were raised. He was provided written and informed consent.
The patient was brought to the operating room. Their identity was verified. General anesthesia was induced, and they were intubated by the anesthesia service. Respiratory and cardiac monitoring leads were placed.
Neuromonitoring leads for somatosensory evoked potential and EMG were placed, and baseline signals were obtained. Foley catheter was placed, which was difficult to pass. They received preoperative prophylactic IV antibiotics and tranexamic acid via IV infusion for hemostasis.
She was positioned prone on the Jackson Relton-Hall frame. All pressure points were carefully padded. Lumbar area was prepped, cleaned with chlorhexidine. A 23-gauge spinal needle fluoroscopy was localized at L5-S1. Skin was sterilized with DuraPrep solution.
A midline incision was demarcated. Sterile drapes were placed in the usual manner. 1% lidocaine with epinephrine was infused.
Skin was opened with a 10-blade scalpel. Hemostasis was obtained with a bipolar electrocautery.
Bovie monopolar was used to carry the incision down through the midline subcutaneous tissues sharply dividing the fascia, and subperiosteal dissection with Bovie and Cobb elevators were performed exposing posterior elements of the spine at L4, L5, and S1 including bilateral transverse processes of L4 and L5, and bilateral S1 ala. During exposure, there was a small incidental durotomy noted at S2-S3 level.
Exploration was performed with curettes and there was a midline sacral defect where the durotomy occurred. This was repaired primarily with a single 4-0 Nurolon stitch and DuraSeal without any further cerebrospinal fluid leakage or issue apparent.
Valsalva maneuver was apparent to verify adequate repair. Next, self-retaining retractors were placed. Woodson elevator was placed under the L4 lamina.C-arm unit was draped sterilely and brought to the field, needed to confirm the level.
Schanz pins were placed in the right posterior superior iliac crest after infusing local anesthesia and creating stab incision with a 15-blade scalpel. The Schanz pins were placed. Neuronavigation was arrayed.
The patient was draped sterilely. Intraoperative CT scan was obtained and the data was transferred to the neuronavigation computer. Accuracy was verified and neuronavigation techniques were used to place pedicle screws in the L4, L5, and S1 pedicles bilaterally.
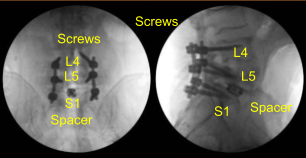
We began decorticating with an electric high-speed drill and Leksell rongeur, cannulated the pedicles of L4 bilaterally with the navigated pedicle finder, palpated for breaches and measured the depths. We used a 5.0-mm tap and placed 6.0 x 45 mm titanium pedicle screws using navigation without difficulty.
Next, we placed the bilateral S1 pedicle screws in the same manner using neuronavigation techniques. Four starting points and trajectory identification, cannulation of the sacrum, we palpated, we under tapped by 2-mm using 5.0 tap and then we placed 7 mm x 40 mm screws without difficulty. Neuromonitoring signals were stable. We did not put the L5 screws at this point.
We began the laminectomy and decompression. We began with the L5 decompression, bilateral pars defects were identified as per the preoperative imaging. Leksell rongeur, Kerrison rongeurs, and electric high-speed drill were used to perform L5 laminectomy and facetectomy was performed which was complete on the left side including the inferior articular process and the superior articular process.
Epidural bleeding was controlled with bipolar electrocautery, surgical hemostatic matrix, and thrombin-soaked Gelfoam.n Copious amounts of sterile irrigation were used throughout the procedure. The L5 nerve root was identified, completely neurolyzed with Kerrison rongeurs and nerve hooks then confirmed with Woodson elevator.
In order to access the L5-S1 disc space, we had to remove the entirety of the L5 and S1 facet on the left side, part of the pedicle, and performed L4 laminectomy.

Nerve root retractor was used to retract thecal sac and S1 nerve root medially towards the patient’s right side. Due to the spondylolisthesis and collapse, which appeared to be worse on the CT scan with bone-on-bone. We had to perform resection of sacral promontory on the left side exposing with Bovie using Kerrison rongeurs and osteotomy to pass through the posteroinferiorly corner of the L5 body, which was collapsed on the sacral endplates.
We used sequential paddle shavers to distract L5-S1 and perform a discectomy. Residual disc material was removed with pituitary rongeurs. Curettes and rasps were used to decorticate the L5 and S1 endplates.
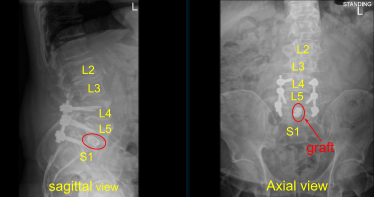
The interspace was irrigated clear. Morselized autograft was packed in the interspace, and then a titanium 22-mm long expandable interbody spacer was gently tamped into the interspace with a mallet. AP and lateral fluoroscopy was performed to confirm midline positioning and depth; the cage was expanded to the appropriate tightness and tight.
X-rays were repeated to confirm correct positioning and size. Neuromonitoring signals were stable. Next with the left L5 pedicle completely isolated and exposed, we placed left L5 pedicle screw decorticating with electric high-speed drill cannulating with the curved freehand Lenke pedicle finder palpating for breaches using 5.0 mm tap and placing 45 mm x 6.0 diameter titanium pedicle screw without difficulty.
We then similarly placed a right L5 pedicle screw as well using similar technique. We draped the patient sterilely and obtained an intraoperative CT scan which showed correct positioning of all the pedicle screws and interbody spacer.
Subsequent to that, we decorticated the bilateral L4-L5 transverse processes and sacral ala for arthrodesis using electric high-speed drill. We confirmed hemostasis with Aquamantys and bipolar. We irrigated the wound clear.
Precut and precontoured titanium rods were selected and placed across the tulips and secured with locking caps, which were all final tightened with torquing and anti-torque devices at L4, L5 and S1. Morselized demineralized bone matrix autograft collected from the decompression as well as bone morphogenic protein allograft were packed into the lateral gutters from L4 to S1 to the posterolateral arthrodesis.
We took final AP and lateral x-rays, which showed correct positioning of all the hardware. The closure will be dictated separately. At the end of the case, the patient was turned supine on the cart, and transported to the recovery room in stable condition.
All sponge counts, needle counts, and instrument counts were correct, and the patient tolerated the procedure well with 250 mL of estimated blood loss. No complications aside from very small incidental S2 approximate level durotomy repaired primarily.
The patient followed up 10 weeks after the surgery for a routine postoperative visit with no complications or signs of infection. Since then the patient has been able to return to their daily activities. Severe radiculopathy and back pain has improved along with no more foot drop syndrome observed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
