Case Study: L5-S1 Transforaminal Lumbar
Interbody Fusion with Interbody Arthrodesis
The patient presented to the neurosurgery clinic with signs and symptoms of lumbar spondylosis and radiculopathy at L5-S1 level of their lumbosacral spine. They failed extensive conservative measures and surgery is recommended to decompress and stabilize their lumbar spine.
The risks, benefits, alternatives, and potential complications were explained to them, and all their questions were answered until no further issues were raised and they provided written informed consent which was placed in the chart.
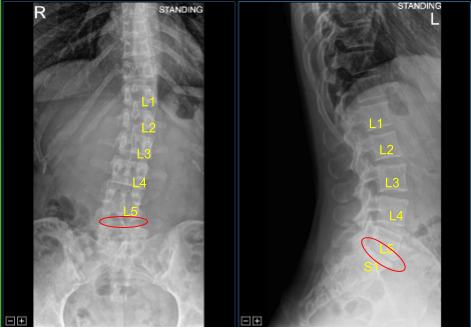
Moderate Disc Degeneration
The patient was brought to the operating room. Their identity was verified. Time-out was performed. General anesthesia was induced, and they were intubated by the anesthesia service. Respiratory and cardiac monitoring leads were placed.
Neuromonitoring leads for somatosensory evoked potential and EMG were placed. They received preoperative prophylactic IV antibiotics. She was positioned prone on a Jackson Relton-Hall frame with all pressure points carefully padded.
Lumbar area was prepped with chlorhexidine and DuraPrep solution. Sterile drapes were placed in the usual manner. 1% lidocaine with epinephrine was infused over the iliac crest.
Two stab incisions were made with 15-blade scalpel. Schanz pins were then tamped into the iliac crest. Neuronavigation array was placed. The patient was draped. Intraoperative CT scan was obtained, and data transferred to the neuronavigation computer.
Accuracy was verified. Neuronavigation techniques were used to identify starting points for bilateral linear incisions which were approximately 4 cm from midline and approximately 2 to 3 cm in length.
The C-arm unit was draped sterilely and used for placement of hardware and localization. We began on the patient’s right side where the incision was infused with 1% lidocaine with epinephrine. Skin was opened with a 10-blade scalpel. Hemostasis was obtained with Bovie.
Bovie was used to sharply divide the fascia. Neuronavigation techniques were used to place a self-drilling, self-tapping titanium pedicle screw into the right L5 pedicle without difficulty due to sclerosis.
Navigated Jamshidi needle was used to cannulate the right S1 sacral pedicle. Jamshidi needle was removed, and a cannulated titanium pedicle screw was inserted with K-wire and then the K-wire was removed. Pedicle screw was also navigated.
Next, we turned our attention to the left side. Again, an incision was infiltrated with local anesthesia and opened with a 10-blade scalpel. Hemostasis was obtained with Bovie and the fascia was divided with Bovie. The navigated Jamshidi needle was placed. We placed K-wire into the left L5 and S1 pedicles and these were clamped down with hemostats and drapes.
C-arm unit was brought into the field and sequential dilators were used to dock the tubular retractor over the left L5-S1 facet joints. Tubular retractor was affixed rigidly to the bed frame with the adaptor arm. Operative microscope was balanced, draped sterilely and brought into the field.
The remainder of the procedure was performed using microsurgical instruments and techniques which were for the purpose of the decompression, neurolysis, and interbody fusion.
Electric high-speed drill with sterile irrigation was used to perform left L5-S1 facetectomy. Hemostasis was obtained with bipolar electrocautery and bone wax.
Navigation was used to guide the trajectory to Kambin’s triangle. Exiting left L5 nerve root was identified, appeared inflamed, was fully neurolyzed with Metzenbaum-Penfield technique and confirmed with nerve hooks.
Annulotomy was performed with 15-blade scalpel, shucker and sequential paddle shavers along with angled and straight micro pituitary rongeurs were used for discectomy. Endplates were prepped with wraps for the arthrodesis. Interbody space was irrigated clear.
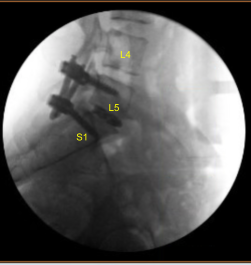
Morselized autograft selected during the decompression as well as morselized allograft was funneled into the interspace with funnel and tamp and then titanium interbody spacer was gently tamped into the interspace under fluoroscopic guidance and expanded into proper position. AP and lateral fluoroscopy showed appropriate positioning.
Next, additional CT scan was obtained showing slightly medial position of the left L5 guidewire. Therefore, Jamshidi navigation was again used to re-cannulate the left L5 pedicle into optimal position. the cannulated navigated pedicle screws were placed over the K wires and K wires were removed with at left L5 and S1 accomplishing a non segmental instrumentation.
The tubular retractor was removed after confirming hemostasis with bipolar electrocautery. Calipers were used to determine size of the pre-cut, pre-contoured titanium rods.
These were placed with inserters across the extender tabs and tulips at bilateral L5-S1 pedicle screws under fluoroscopic guidance and secured with locking caps which were finally tightened with torque and anti-torque device after removing the inserters. Extender taps were removed with the breaker device. Hemostasis again confirmed.
Wounds were irrigated clear. Schanz pins were removed. Vancomycin powder was applied. Bilateral closures were accomplished with 0 Vicryl pop-off interrupted sutures for water- tight closure of the fascia. Exparel long-acting local anesthetic was then infused into the soft tissues to the fascia.
The dermal layers were closed with 2-0 Vicryl sutures. The skin incisions were closed with running 4-0 Monocryl subcuticular sutures, cleaned, dried sterilely, and dressed with Dermabond glue. The Dermabond was also applied for the iliac crest array Schanz pin incisions. We did obtain a final CT scan and final x-rays showing correct positioning of all the hardware.
At the end of the case, sponge, sharp, needle, and instrument counts were correct. The patient tolerated the procedure well. The patient was turned supine on the cart, extubated uneventfully, and transported to the recovery room in stable condition.
The patient followed up a couple of weeks after the surgery and then continued following up in our office 4, 6, 8 weeks. In their last office visit the patient stated that their symptoms of lumbar spondylosis and radiculopathy were resolved. The patient also agreed to continue physical therapy.


Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
